As more patients are discharged from stressed ICUs, they face multiple problems brought on by the pandemic.
1:52 PM
Author |

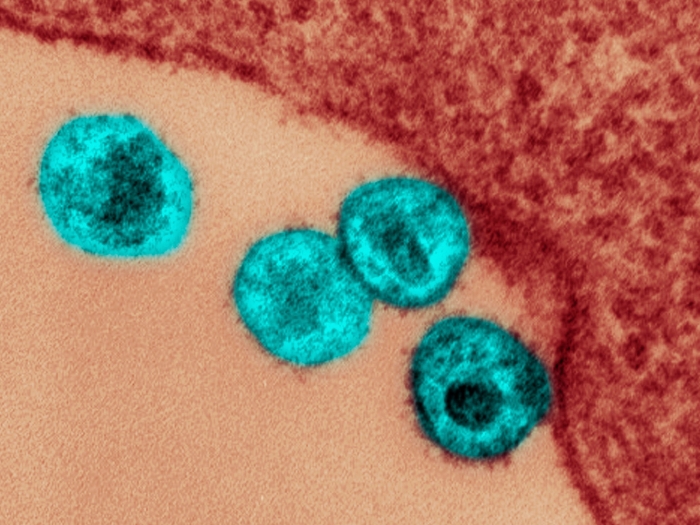
Across the country, intensive care units continue to fill with patients infected with COVID-19. It can be easy to forget in the influx of daily case counts that in each of those beds is a person fighting for their life, aided by a care team working under extraordinary circumstances. In hospitals everywhere, so much of the scene on COVID floors is abnormal: patients heavily sedated; healthcare providers trying to offer comfort while cloaked in stifling personal protective equipment; missing loved ones, who would normally sit vigil at a patients' bedside, kept away by the threat of infection.
According to Michigan Medicine experts who have been studying the downstream effects of critical illness for years, the pandemic will have severe effects on the lives of those who are eventually discharged from the hospital.
"With the virus itself causing severe illness, combined with the challenges of delivering healthcare [for these patients] means that issues after severe COVID-19 may be multiplied, and the time to recovery longer," says Hallie Prescott, M.D., assistant professor of pulmonary diseases and critical care medicine. She notes that existing studies of the aftermath of pneumonia, sepsis and acute respiratory distress syndrome offer clues to what awaits COVID patients. For example, says Prescott, most patients with these illnesses eventually recover their lung function.
Yet many patients report lingering weakness, exercise intolerance and reduced quality of life after an ICU stay. And with COVID, there are many unknowns. "Most studies look at patients up to a year after their illness. We haven't had this around long enough to have those studies coming out."
Even under more normal circumstances, a stint in the ICU often results in physical impairments as well as cognitive impairments, anxiety, depression and post-traumatic stress disorder, says Prescott. All of these symptoms are encompassed under what is known as post-ICU syndrome or post-sepsis syndrome. In a recent review and editorial in the Journal of the American Medical Association, Prescott and her colleagues outline how lessons learned from recovery trends following other critical illnesses offer a roadmap for clinicians taking care of COVID-19 patients.
While some of the post-ICU symptoms can be mitigated by ongoing physical and occupational therapy during hospitalization, the volume of coronavirus cases and the need for infection control and personal protective equipment (PPE) make it difficult to provide to all patients with COVID. That combined with the unknowns specific to COVID, such as potential heart, kidney and other organ damage from the virus, make the prospect of a full recovery after discharge more difficult.
"The incredible number of patients being discharged from ICUs is overwhelming for our system, and these people are often not discharged with the resources they need to continue their recovery, especially as the inpatient systems are struggling with large numbers of complex patients," says Jake McSparron, M.D., assistant professor in the division of pulmonary diseases and critical care medicine.
He says Michigan Medicine's Post-ICU Longitudinal Survivor Experience, or PULSE, clinic, designed to help streamline all of the services a patient might need after the ICU, is now almost exclusively seeing COVID patients since the surge of cases. The Division of Physical Medicine and Rehabilitation has also increased capacity since the pandemic began to offer expanded inpatient and telemedicine appointments for patients recovering from COVID-19.
The path forward after COVID
Missing from the typical recovery equation, Prescott adds, is having family at the bedside. "Family often serves as a huge support to patients, helping them take their medicines, know when their appointments are, and offering support in recovery—but they have not been allowed in the hospital," she says.
And while FaceTime and other video conferencing has allowed family to stay somewhat connected, many are finding discharge instructions more of a struggle to understand.
Prescott is collaborating with a team from the Biosocial Methods Collaborative at the U-M Institute for Social Research to do a deeper dive into family caregiving for critically ill patients. What began with a focus on any patient who had been in the ICU before the pandemic has now transformed into a study of COVID's effect on patients and their families, called HEART, short for Health Enhanced by Adjusting and Recovering Together. Working with an interdisciplinary team of faculty and staff from critical care, social work, nursing and psychiatry, they hope to more fully understand the pressures on COVID informal caregivers and care receivers through interviews and submitted personal stories.
"So far we're learning that caregivers feel they've been ripped out of this place they wanted to be, they wanted to sit bedside, they don't have the information, they're told to go to primary care and primary care doesn't know what to do," says Alicia Carmichael, a research process director with the collaborative. "Then there's the stigma of being exposed to COVID. From what we can tell, they're really struggling."
The team is actively seeking COVID survivors, whose contributions they hope will inform care and support for caregiving going forward.
Other research led by John Scott, M.D., assistant professor of surgery, will look at long term outcomes for survivors of severe COVID-19, to understand if and how they get their lives back after discharge. "Making it through a tough hospital course is just the start of the journey to recovery," Scott says. "The ultimate goal of our planned study is to design interventions—medical, social, economic—to help patients not only survive after COVID, but thrive."
Paper cited: "Recovery from Severe COVID-19: Leveraging the lessons of survival from sepsis," JAMA. DOI: 10.1001/jama.2020.14103

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!