A new study finds only half of women who could benefit from genetic testing get it, and often not before they have surgery.
4:00 PM
Author |
As new genes are linked to breast cancer occurring in families, and as genetic testing becomes more important in directing treatment for newly diagnosed patients, a substantial number of those at the highest risk are not getting tested.
MORE FROM THE LAB: Subscribe to our weekly newsletter
Nearly half of newly diagnosed breast cancer patients who should be recommended for genetic testing did not get it. A quarter of these patients were not counseled about their potential risk, a new study finds.
Among those who were tested, fewer than two-thirds met with a counselor before surgery, when results could most influence treatment.
The University of Michigan study is published in the Journal of Clinical Oncology.
When a woman with a family history of cancer gets diagnosed with breast cancer or when a woman is diagnosed at a young age, it could suggest she has a genetic predisposition for breast cancer. About a third of breast cancer patients fall into this category.
For those who test positive, a genetic link might change their treatment path. For example, women might choose to have double mastectomy if testing indicates they are at high risk of a second breast cancer.
"Integrating genetic counseling into treatment decision-making is challenging. Oncologists appropriately focus on treatments for cancer that's been diagnosed, and patients often desire to make decisions quickly. Addressing the risk of secondary cancers from a hereditary risk may be seen as a lower priority," says study author Steven J. Katz, M.D., MPH, professor of general medicine and of health management and policy at the University of Michigan.
Making matters more complicated are new multigene panel tests that look at 25 to 40 genes. Physicians don't know the impact of some of these genes. In some cases, testing can identify a so-called variant of unknown significance — in other words, the gene is altered, but it's not clear if that alteration contributes to cancer risk.
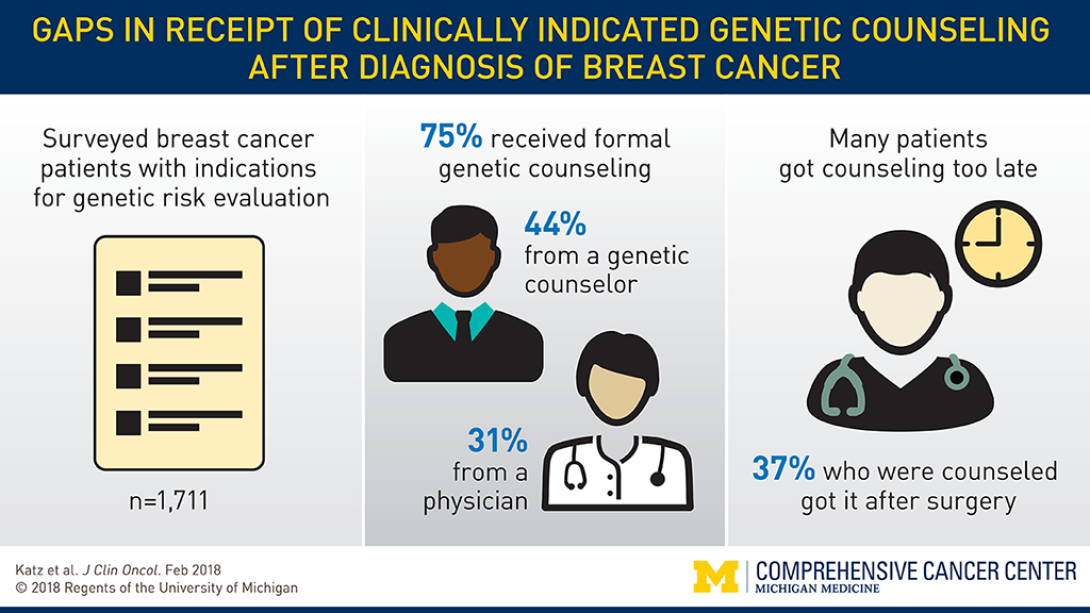
Researchers looked at surveys from 1,711 women newly diagnosed with early stage breast cancer for whom genetic testing is recommended. Patients were asked if they had discussed a genetic test for breast cancer risk and whether they had met with a genetic counselor.
SEE ALSO: Genetic Sequencing Can Influence Treatment for Advanced Cancer
Overall, three-quarters of the patients reported receiving some form of counseling, from either a genetic counselor or their physician. But counseling was much more common among those who chose to have testing: Nearly all the patients who had genetic testing also had counseling. For those in this high-risk group who did not get tested, only half reported having counseling.
"It appears a substantial minority of patients do not receive any form of genetic counseling, highlighting a significant unmet need," Katz says.
Not every woman who receives genetic counseling will decide to undergo testing. But, Katz stresses, information — and the timing of the discussion — are important to making informed treatment decisions.
"Patients should get counseling before surgery. Bilateral mastectomy is a risk-reducing surgical option for those who test positive. Women need to be able to consider that in the context of their surgical treatment decision. Our study found that counseling too often does not come quick enough," Katz says.
"We need to find new ways to better integrate genetic counseling into practice by incorporating different clinicians, including genetic counselors, more flexibly and giving them tools to help patients understand the implications of testing on their treatment," says senior study author Sarah T. Hawley, Ph.D., MPH, professor of internal medicine at Michigan Medicine.
Read the research papers about cancer and decision-making published by members of Cansort, the Cancer Surveillance and Outcomes Research Team.
Learn more about the University of Michigan's Cancer Genetics Program https://www.rogelcancercenter.org/cancer-genetics.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!