Study: Sepsis costs a total of $7.3 billion and disproportionately impacts vulnerable kids.
6:34 AM
Author |

When a child's immune system responds to an infection, it can sometimes cause damage to vital organs – which can result in long hospital stays and invasive interventions and procedures.
This life-threatening condition, known as sepsis, is a leading cause of death among children and newborns. And now a new study suggests it may also be among the costliest types of hospitalizations for kids.
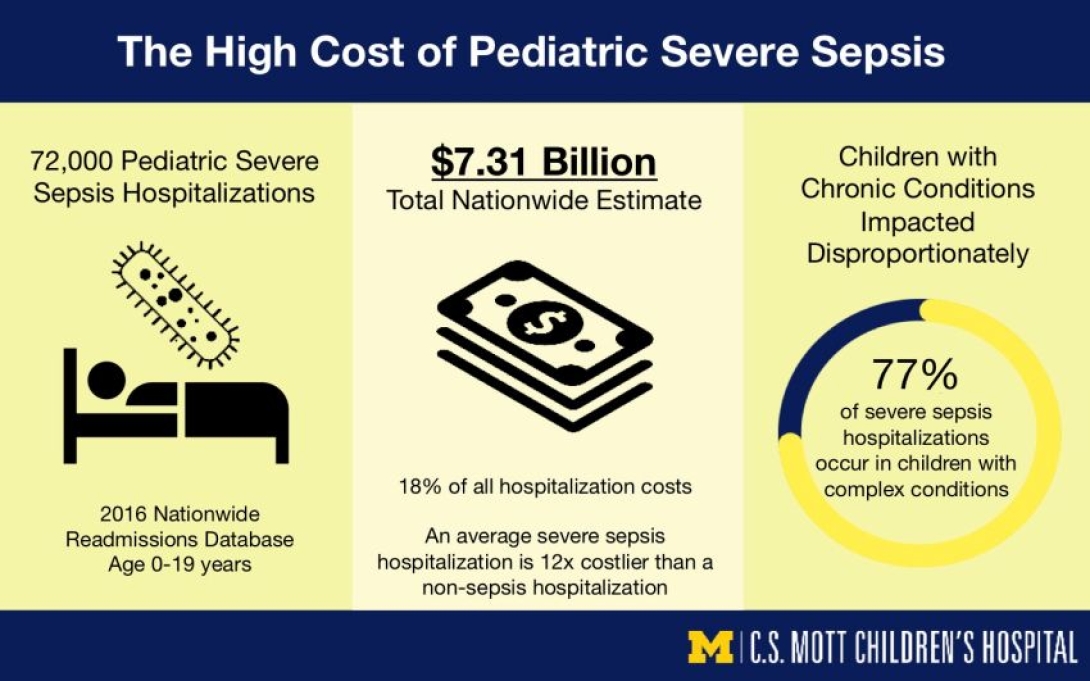
Michigan Medicine researchers analyzed national data suggesting pediatric severe sepsis hospitalization cost roughly $7.3 billion among an estimated 72,288 hospitalizations in 2016 – with costs disproportionately impacting vulnerable children with complex chronic conditions.
Overall, a single pediatric severe sepsis hospital stay costs $26,592 – 12 times the average of all other pediatric hospitalizations according to the findings published in JAMA Pediatrics. But this number is likely "just the tip of the iceberg" says lead author Erin Carlton, M.D., a pediatric intensivist at University of Michigan C.S. Mott Children's Hospital.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily updates on iTunes, Google Play and Stitcher.
While acute inpatient care of severe sepsis is associated with nearly one-fifth of all hospitalization costs among U.S. children, Carlton notes that this likely underestimates total costs because they don't include post-hospital costs or lost work among caregivers.
"Our study sheds light on the prevalence and high expense of pediatric severe sepsis," Carlton says. "Sepsis is common, costly and is taking an increasingly heavy toll on patients, families and the healthcare system."
Almost 7,000 children die from severe sepsis a year, previous studies suggest. And those who survive the condition may suffer from long-term health issues, including disability.
Sepsis is common, costly and is taking an increasingly heavy toll on patients, families and the healthcare system.Dr. Erin Carlton
Sepsis happens when the body's response to infection goes into overdrive, causing collateral damage to other organ systems. Children, especially infants and those with underlying medical conditions, are at particular risk for sepsis.
Unvaccinated babies and children are also susceptible to such infections, especially under age three when the immune system is not yet fully developed. Infections can also be passed from mother to child during pregnancy, labor, and delivery.
Sepsis costs disproportionately impact vulnerable kids
Children with complex chronic conditions account for about three quarters of pediatric severe sepsis hospitalizations, Michigan Medicine researchers found. This group faces long-term medical conditions that require specialty pediatric care and often inpatient hospitalization.
In the study, children with at least one complex chronic condition accounted for 77% of severe sepsis hospitalizations but more than 90% of total hospitalization costs, suggesting this vulnerable population and their families endure a disproportionate burden of severe sepsis.
"There has been a growing focus on the impact of critical illness, like severe sepsis, on children with complex chronic conditions," says Carlton, who is also a researcher with the U-M Institute for Healthcare Policy and Innovation and Susan B. Meister Child Health Evaluation and Research Center.
Sepsis quickly progresses from mild to severe stages, but early symptoms can be difficult to identify, especially in children, leading to delays in diagnosis and effective treatment.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Some hospitals have rolled out protocols to quickly identify signs of sepsis and respond with high levels of coordination among care teams. As part of the Improving Pediatric Sepsis Outcomes Collaborative by the Children's Hospital Association, Mott has implemented a sepsis response team to quickly identify children admitted to the hospital or in the emergency department who may have sepsis and facilitate swift intervention.
Carlton says further studies are necessary to get a full picture of costs and how health providers can continue to improve sepsis care.
"We need to expand research on how this condition is affecting children and their families as they're discharged from the hospital and returning to their communities. Are these higher costs following them? And if so, are there ways to streamline the process and better support patients and families through their post-sepsis care?" Carlton says.
"Early recognition and treatment of sepsis are key to a recovery with good outcomes," she adds. "If we can use protocols that help us recognize sepsis early and treat it more quickly, then we can reduce the length of hospital stays, lower healthcare costs and improve outcomes for children and their families."
Paper cited: Carlton, E., Barbaro, R., Iwashyna, T., Prescott, H. "Cost of Pediatric Severe Sepsis Hospitalizations" JAMA Pediatrics. DOI: :10.1001/jamapediatrics.2019.2570

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!