Survey of 20 centers nationwide reveals impacts of reduced services.
5:00 AM
Author |

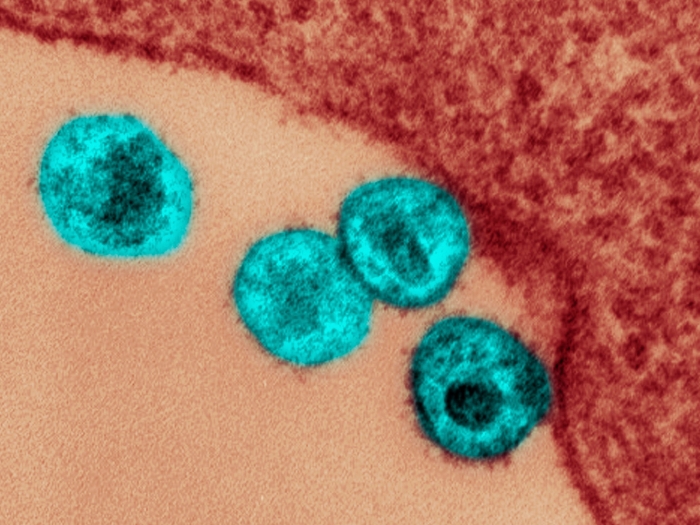
When the COVID-19 pandemic arrived in North America in March 2020, health care facilities stopped providing all but "essential" care, to reduce infection risks and preserve protective gear known as PPE.
That included changes at many centers that provide ECT, or electroconvulsive therapy, for severe depression and other conditions, the survey shows.
Because ECT involves anesthesia, so that patients are unconscious when carefully controlled pulses of electricity are delivered to key areas of the brain, it is considered an 'aerosol generating' procedure – posing special risks when a respiratory virus such as the novel coronavirus is in widespread circulation.
In a new commentary in the American Journal of Psychiatry, a team led by Daniel Maixner, M.D., of the University of Michigan Department of Psychiatry and U-M Eisenberg Family Depression Center, describes the experiences of ECT centers during spring of 2020. Maixner leads the ECT program at Michigan Medicine, U-M's academic medical center.
Like Podcasts? Add the Michigan Medicine News Break on iTunes or anywhere you listen to podcasts.
Some centers temporarily stopped accepting new patients for ECT, or prioritized ECT care, for only the most severely ill and hospitalized patients. Many changed the schedule for the repeated treatments that a course of ECT entails. All followed newly developed protocols to reduce staff exposure to aerosols using patient screening, used advanced personal protective equipment, also called PPE, and collaborated extensively with anesthesia teams to safely administer treatments.
SEE ALSO: ECT Emerges as Cost-Effective for Treatment-Resistant Depression
In all, 16 of the centers reduced their capacity to less than half of their usual patient volume between March and June, including five that treated less than a quarter of their usual number of patients. For new patients, and those who had completed their initial course of treatment but needed maintenance, 18 of the 20 centers reduced the frequency of treatments.
The changes came with a price. One center lost a patient to suicide. Three other centers had patients who made serious suicide attempts. Seventy percent of sites had patients return to inpatient psychiatric care after living in the community because they weren't able to receive ECT on the planned schedule, and 80% of the centers had patients who had to restart ECT care from the beginning to get back on track.
It is important for psychiatrists and patients to advocate for ECT to remain an essential treatment and not just be considered elective.Daniel Maixner, M.D.
Because of this, the authors call for ECT to be seen as "essential" in future waves of COVID-19 activity, and in other crises and pandemics, so that care can continue.
With improved availability of COVID testing and PPE, and treatment protocols, most of the academic ECT programs were able to react promptly and return to caring for most patients again by mid-summer 2020, despite many challenges.
However, Maixner says, "risks are high for our patients during the time of COVID-19 and any other pandemic if access to ECT is curtailed. It is important for psychiatrists and patients to advocate for ECT to remain an essential treatment and not just be considered elective."
SEE ALSO: COVID Forced Psychiatric Care Online, and Many Patients Want It to Stay There, Study Finds
The survey was conducted by the ECT Task Group of the National Network of Depression Centers. In addition to the new commentary, Maixner presented additional data on the effects of the pandemic on ECT practice at a recent meeting of the International Society for ECT and Neurostimulation, which has also issued a position statement on the essential role of ECT.
Maixner and colleagues have also studied the efficacy and cost-effectiveness of ECT as a key option for patients who have not responded to other forms of treatment for depression and other mental health conditions.
Paper cited: "Electroconvulsive Therapy Is an Essential Procedure, Am. J. Psychiatry," American Journal of Psychiatry. DOI: 10.1176/appi.ajp.2020.20111647

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!