There are no therapies proven to prevent or treat COVID-19 yet, but providers can help address symptoms while they continue researching new ideas.
11:27 AM
Author |
Editor's note: Information on the COVID-19 crisis is constantly changing. For the latest numbers and updates, keep checking the CDC's website. For the most up-to-date information from Michigan Medicine, visit the hospital's Coronavirus (COVID-19) webpage.
Interested in a COVID-19 clinical trial? Health research is critical to ending the COVID-19 pandemic. Our researchers are hard at work to find vaccines and other ways to potentially prevent and treat the disease and need your help. Sign up to be considered for a clinical trial at Michigan Medicine.
Although most people can stay home while they recover from the novel coronavirus, people who are having trouble breathing sometimes require a hospital stay.
And for now, a focus on those difficult symptoms, like being unable to breathe, is what hospitals like Michigan Medicine offer their COVID-19 patients. Providers are giving treatments to address symptoms and support patients so that their bodies can best fight the infection and begin to heal.
That's because there are no tested therapies proven to prevent or treat COVID-19.
"Our clinicians, physician-scientists, other researchers at Michigan Medicine and the University of Michigan are already actively gearing up to explore treatments and better understand how best to treat this disease and who's at risk for it," says Daniel Kaul, M.D., an infectious disease expert at Michigan Medicine. But until better scientific data is available, hospital caregivers have no proven antiviral therapy to offer.
Here, Kaul and Michigan Medicine's chief of hospital medicine, Vineet Chopra, M.D., M.Sc., address the latest questions they're frequently seeing about treatment for COVID-19, and what may be on the horizon as research continues.
And although they describe some potential therapeutic and treatment options that are being explored, both warn against seeking out these drugs on your own or trying other untested remedies. Kaul and Chopra say it's important to allow your health care provider to evaluate your individual situation to provide the best recommendation for you.
Should people with COVID-19 take chloroquine or hydroxychloroquine? Do you prescribe them to your patients with COVID-19?
Michigan Medicine just changed its guidelines on prescribing these drugs. There's a lot of excitement about whether these already existing options for malaria could be useful in COVID-19, but so far that excitement hasn't materialized in patient care data.
"Our infectious disease division and our antimicrobial pharmacists have reviewed all the available data and we found no convincing evidence that these drugs were effective in treating people with COVID-19," Kaul says.
That's consistent with what's been observed firsthand in Michigan Medicine's hospitals.
"We haven't seen any clear evidence of benefit so we aren't going to use hydroxychloroquine routinely anymore," Chopra says. "We were initially recommending it to both inpatients and outpatients, but we're no longer doing that routinely. That's based upon the fact that we've been prescribing hydroxychloroquine for a few weeks, did not see therapeutic benefit, but did see adverse effects."
Those side effects Chopra has seen in his patients include liver function toxicity, nausea and vomiting.
Moving forward, Chopra and Kaul say the strategy is to individualize these decisions for each patient, considering risks and benefits based on that person's health history and symptoms.
Chopra notes that use of chloroquine or hydroxychloroquine could also exclude a patient from being allowed to join other COVID-19-related clinical trials, so it's important to consider all of these factors before prescribing the drug.
How will we eventually get an effective COVID-19 treatment or prevention option?
"Given there's no proven treatment thus far, the ideal circumstance is to enroll as many people as possible in clinical trials so we can offer people treatments that may have direct benefit to them and to figure out what works," Kaul says, "because that's the only way to figure out what works: do a proper clinical trial."
Providers at Michigan Medicine are involved in several clinical trials, working to figure out how to offer people dealing with COVID-19 better options.
"All of the drugs we're giving here are being administered in the context of clinical studies," Chopra says. "We want to know what works because the numbers support that determination: fact, not fiction. This will help us inform the care of patients here and around the world, using the best scientific principles."
For example, scientists are studying whether a class of drugs typically used to control inflammation and reduce complications in transplant patients could help prevent lung damage in COVID-19 patients.
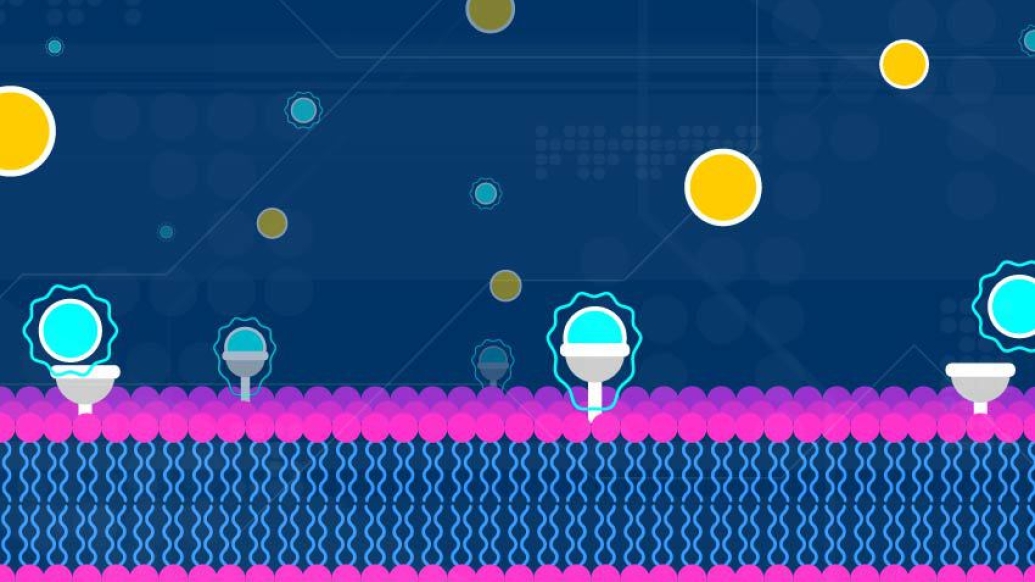
"These interleukin 6 inhibitors target one specific cell where we think much of the harm happens in patients with COVID-19," Chopra says. "Current clinical trials are investigating whether a specific dose or timing would have the most benefit. The IL-6 blockers, including sarilumab and tocilizumab, are promising and I think we'll see more of their use in COVID-19."
Plasma therapy, another topic appearing in the media lately, is also an intriguing option that's being explored, Kaul says.
Kaul says it's important to know that providers are treating each patient individually, and making individual recommendations regarding the best option to improve people's symptoms and help them leave the hospital quicker. Your doctor is the best person to talk to about what other options might help you feel better if you are dealing with severe COVID-19 symptoms, he says.
Why is there worry about taking ibuprofen if you think you might have COVID-19?
Kaul says there are theoretical reasons ibuprofen or other NSAIDs could make a person more susceptible to having a more severe experience with COVID-19. That being said, it's all theoretical at this point.
"We don't really see a downside to using Tylenol, though, which doesn't have those theoretical risks," he says. "Our general thinking is, 'Why not use Tylenol, because almost no one who can take ibuprofen can't also take Tylenol.'"
Be sure to read and heed the dosages and intervals between doses on the package, and the warnings about interactions with alcohol and other drugs.
However, if you are having trouble breathing or dealing with other severe symptoms, Kaul recommends you call your primary care doctor for advice, or go in to be seen if severe.
Should I call or stop in to see if I have COVID-19?
Although test turnaround time and availability continue to improve, both physicians say the reason to contact a provider about COVID-19 is if you're feeling bad enough to need medical help. Supplies like swabs and chemicals are limited, so the general public can't be tested at this time.
"We recommend people who have symptoms consider themselves infected," Kaul says. "If you're not feeling short of breath, but feel particularly flu-ish and don't have a lot of medical problems, the general rule is to stay home and call your primary care physician if you have concerns."
What's your takeaway message for people worried about COVID-19?
Chopra says his advice is the same it's been for a few weeks now:
"The best treatment for this disease is to not get it, and the way you don't get it is by staying at home," he says. "The only way to stop the cycle is to prevent transmission from people who are asymptomatic. Even if it's brief, every time we come in contact with others we are taking a risk. Keep in mind, the virus has a long incubation period before symptoms appear."
Kaul says while there are no proven treatments, the supportive care, meaning respiratory and other help, can be the difference between life and death for some patients.
"We don't want people to think there's nothing we can do. If you have significant shortness of breath, dizziness or other concerning symptoms, talk to a medical professional or come in," he says.
And if you're feeling sick with symptoms suggestive of COVID-19, both doctors encourage you to seek help from a medical professional instead of trying any untested remedies at home.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





