The same approach that helps patients manage powerful blood thinners could help expand access to medication-based addiction treatment.
7:00 AM
Author |
More than 2 million Americans need help with an addiction to opioid painkillers or other opioid drugs. For many, that help could come in the form of a medication called buprenorphine.
SEE ALSO: Why U.S. Doctors Hate Marijuana and Love Opioids for Chronic Pain
But doctors need special permission to prescribe it. And with that permission comes the understanding that every patient who gets the drug needs regular urine tests, dosage checks and adjustments, and counseling for months or even years.
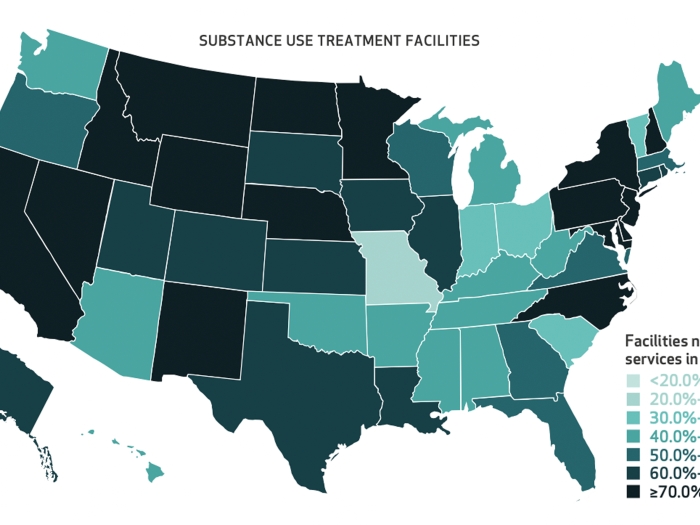
Because most primary care doctors don't have the means to provide this intensive level of care, the number of clinics offering the medication stays low — keeping a proven opioid addiction treatment out of reach for many who need it.
The answer to this predicament, a trio of University of Michigan Medical School opioid researchers says, could lie in an entirely different area of medicine — one that tries to prevent strokes, not drug overdoses.
In a recent article in the journal Addiction, they argue the same approach used with patients on powerful blood-thinning medications could help many individuals who may benefit from buprenorphine for opioid addiction.
Millions of people receive blood-thinning medications, or anticoagulants, such as warfarin, to manage their risk of strokes and other problems related to blood clots. They need frequent blood tests, dosage checks and adjustments, and counseling about diet and risky behaviors over many months or years to manage their risk of clotting or uncontrolled bleeding.
This intensive care often comes not from the prescribing physician, but from anticoagulation clinics with teams of nurses, pharmacists and nurse practitioners. The country has nearly 3,000 such clinics, which serve nearly a million patients a year.
The same setup could work for buprenorphine, for patients who are stable enough to receive the drug on an outpatient basis, says first author Pooja Lagisetty, M.D., M.Sc., a research investigator at U-M and member of the Institute for Healthcare Policy and Innovation.
Lagisetty is one of only 500 doctors in the state of Michigan licensed to prescribe the drug. She will be prescribing it at the VA Ann Arbor Healthcare System.
Together with opioid addiction researcher Amy Bohnert, Ph.D., MHS, and chronic disease management expert Michele Heisler, M.D., MPH, Lagisetty also proposes that doctors who prescribe opioid painkillers could use the same approach to make sure patients get effective pain care without addiction.
What's more, they say, many anticoagulation clinics are facing a drop in demand, thanks to a new class of blood thinners. Patients taking them need less testing and counseling than those taking warfarin — so the timing may be perfect for a resource shift.
Do we turn our heads and not treat them, or do we learn how to do it better?Pooja Lagisetty, M.D.
Improving access to buprenorphine
"On average, most physicians who have permission to prescribe buprenorphine are treating 13 patients with it," Lagisetty notes.
SEE ALSO: Opioids: When the Harms Outweigh the Benefits
By law, they can prescribe to a maximum of 30 in the first year. After that, it's as many as 275 patients annually — a figure raised from 100 earlier this year.
"A big part of the reason is because it's so labor-intensive to care for these patients, especially during the induction or initial phase of treatment, but even through maintenance therapy," Lagisetty explains. "As a primary care physician, I already rely on pharmacist- and nurse-led teams to manage my patients on anticoagulants. Could we do the same for buprenorphine, or even opioid pain treatment?"
Even if the country's 7,200 approved buprenorphine prescribers started referring just the patients who have the highest risk of relapse and the most intense needs to pharmacists and nurses, it could free up time to take on more opioid-addicted patients, she says.
She cites a five-year study from a Boston University team that showed that half of buprenorphine patients seen in a clinic with nurse-managed care had successful treatment after a year — and that nearly all patients who stuck with the treatment for a year were completely off illicit drugs including heroin and cocaine.
"This may be the only way to get more physicians who don't have buprenorphine prescribing waivers to buy in — to show that collaborative care is working," says Lagisetty. "We already have the existing infrastructure; we need to train the providers who are used to medication management and say 'Here's a new medication to manage.'"
Of course, she and her colleagues acknowledge, the complexities of addiction are different from those of stroke risk. After all, addiction carries a societal stigma, and blood thinning does not.
Plus, tapering a buprenorphine dose requires shared decision-making by providers and patients, so providers would need training in techniques such as motivational interviewing, which Bohnert and her colleagues have shown can help patients reduce risky opioid use.
But with so many Americans using opioid painkillers, and a sizable percentage of them becoming addicted, the time to act is now, the U-M team says.
Lagisetty says doctors who take on the responsibility for prescribing buprenorphine must also learn how to identify the patients who will do the best: those motivated to quit opioids with the help of medication, who keep regular appointments and who can follow the medication guidelines. The more support clinics can offer them, the better they will do.
The current national epidemic, and the changes in buprenorphine prescribing restrictions and anticoagulation care, make this a crucial time, she adds, asking, "Do we turn our heads and not treat them, or do we learn how to do it better?"

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!