Researchers uncover a mechanism that explains why a Hedgehog inhibitor kills skin cancer, but not completely.
7:00 AM
Author |
What happens when the most common and least threatening type of cancer gets complicated?
MORE FROM THE LAB: Subscribe to our weekly newsletter
A new study pinpoints a mechanism that controls how basal cell cancers respond to treatment and offers new ideas for controlling this disease when it gets tricky.
Basal cell carcinomas are incredibly common — between 1 million and 3 million Americans are diagnosed each year — and rarely life-threatening. They are most often removed through surgery.
But for a small minority of patients, they can be a bigger problem.
In some cases, the cancer cannot be surgically removed, often because of where it's found. A small portion of patients have an inherited condition called basal cell nevus syndrome, or Gorlin syndrome, which causes hundreds of basal cell tumors to develop over their lifetimes.
Enter the drug vismodegib. It's an early success story among targeted therapies, developed to hit a key pathway in basal cell carcinoma called Hedgehog. By blocking Hedgehog, the cancer cells die.
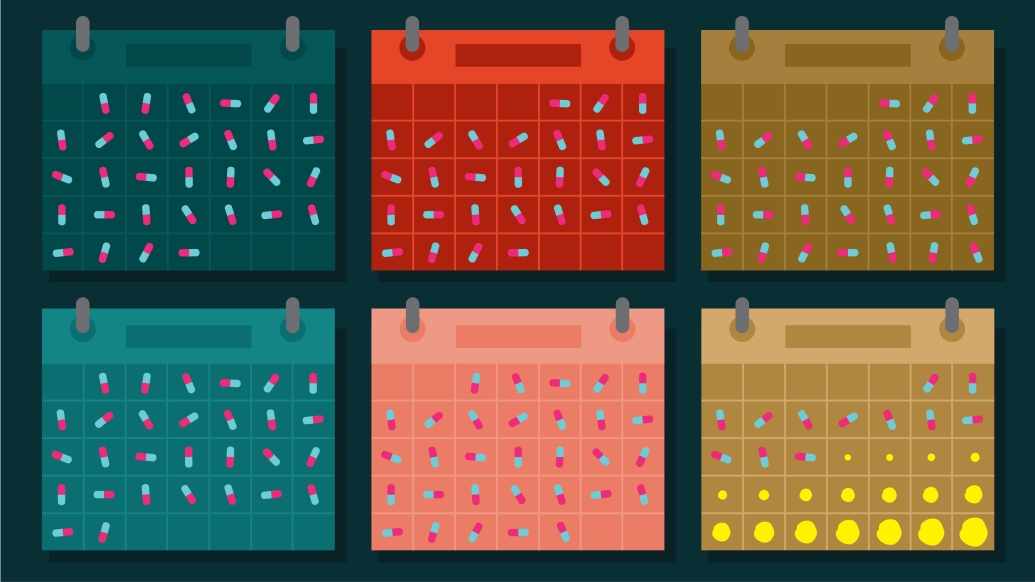
But there's one catch: When patients stop taking the drug, the cancer often grows back at the same site.
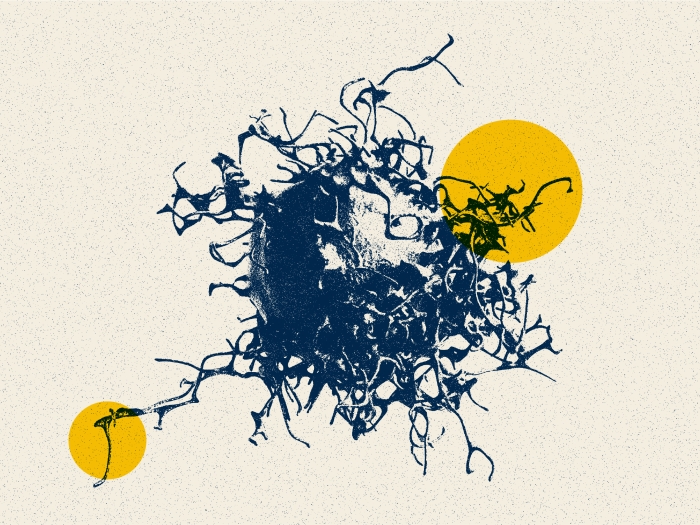
"It's a very effective drug, but many patients have to stay on it for their entire life," says Sunny Wong, Ph.D., assistant professor of dermatology and of cell and development biology at Michigan Medicine. "We think vismodegib drives a subset of tumor cells into a state of dormancy, where they neither grow nor die."
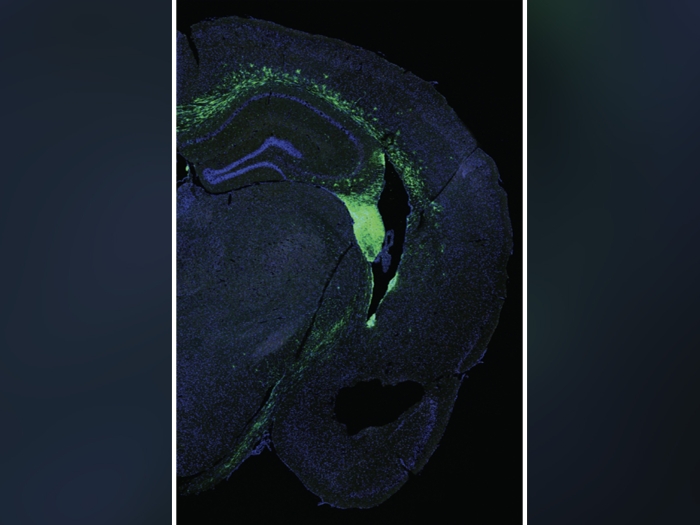
In a study in Cancer Cell, researchers describe two types of cell populations in basal cell tumors. The outer edge of the tumor is lined with cells that persist even in the face of Hedgehog blockade. The inner cells, on the other hand, are about three times more likely to undergo cell death from vismodegib treatment.
SEE ALSO: Detecting When the Most Common Skin Cancer Turns Dangerous
"What was most fascinating was that the relative location of a cell within a tumor can have such a big effect on its sensitivity to drug treatment," says lead study author Markus Eberl, Ph.D., a former postdoctoral fellow at Michigan Medicine.
The difference stems from the Notch pathway and how each type of cell activates it. Higher levels of Notch were detected in the inner cells, while the outer cells had lower levels. When the researchers shut off Notch, tumors were more likely to persist despite vismodegib treatment. When they turned on Notch, tumors shrank. The work was done in mice.
The outer cells are anchored to the tumor's basement membrane, where Hedgehog signaling is high and Notch signaling is low. The researchers explain that this pattern allows cancer cells to persist in a largely dormant state while the patient takes the Hedgehog-inhibiting vismodegib. Once the drug treatment stops, the dormant cells reactivate.
Notch plays a key role in normal skin and is the most common mutation in skin cancers, seen in up to half of patients.
Fewer than 1 percent of patients with basal cell tumors will need vismodegib.
"The side effects of vismodegib are not life-threatening, but there are concerns," Wong notes.
Many patients experience loss of taste, muscle cramps, weight loss and fatigue. The side effects drive some patients to discontinue the drug.
Drug resistance and tumor persistence are both challenging issues with Hedgehog-blocking treatments. This is the first study to address persistence and explain how the drug works and, in some cases, falls short.
"Eliminating persistent tumor cells is necessary to cure patients who have tough-to-treat cases of basal cell carcinoma," Eberl says.
The researchers suggest the key might be in developing a drug that changes the tumor architecture so the persistent outer cells respond more like the inner cells. Additional research is underway into the mechanisms of why Notch affects cell death, searching for proteins or molecules that may be at play.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!