The type of dementia that actor Robin Williams had is a complex disease with ambiguous symptoms. What doctors and patients need to know — and what progress is being made.
2:00 PM
Author |

Lewy body dementia, the third most common form of dementia, perhaps accounting for up to 20 percent of cases, remains a mystery.
Symptoms can overlap with those of other conditions, which might lead to misdiagnosis or potentially harmful medications. And it can be tough to detect through blood tests or brain scans — with the only official confirmation, a brain biopsy, unfeasible until death.
That leaves doctors to connect the dots to identify Lewy body dementia.
For families and physicians alike, "there's a lot of emotional turmoil," says Henry Paulson, M.D., Ph.D., a professor of neurology at the University of Michigan and the director of the Alzheimer's Disease Center at U-M.
In 2014, the suicide of actor Robin Williams, who was later revealed to have the disease, put the condition in the spotlight.
Raising awareness, too, is the Carl Rinne Lewy Body Dementia Initiative at U-M. Established in January, a primary goal of the effort — named in honor of the retired Ann Arbor professor and musician who died from the disease — is, Paulson says, to "really educate the public and health care professionals."
Paulson spoke recently about the disease.
What causes Lewy body dementia?
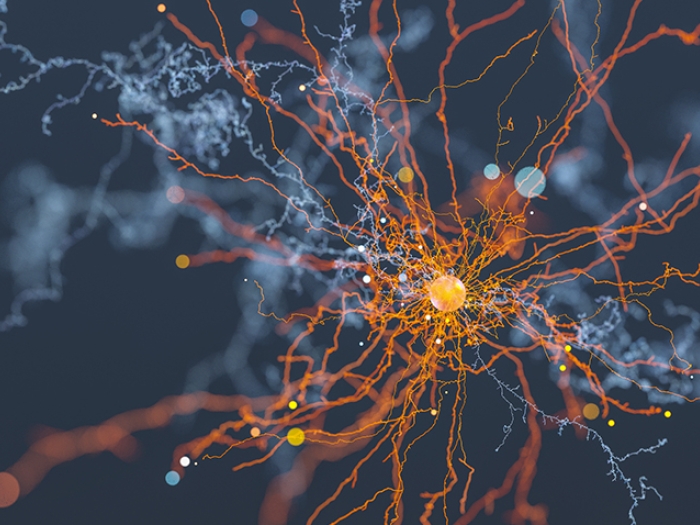
Paulson: As the name implies, there are these small protein accumulations in the brain called Lewy bodies. They are aggregates of a particular protein, alpha-synuclein. They accumulate in the brain and are somehow linked to the psychiatric and cognitive changes that occur.
But we don't yet know how that aggregation contributes to psychiatric and cognitive problems.
How might a doctor first spot trouble?
Paulson: In addition to dementia, which may overlap with some of the features of Alzheimer's, we look for other clues: signs of Parkinson's, such as stiffness or slowness of movement, and visual hallucinations that you don't see often in Alzheimer's patients.
We also look for fluctuating levels of consciousness; good and bad days; periods of lucidness and complete fogginess.
REM sleep disorder is also common. People who have it "act out" their dreams — they murmur, shout or flail their arms while asleep.
Why is Lewy body dementia so commonly misdiagnosed?
Paulson: For a lot of people with cognitive impairment, when doctors think it's dementia they use the word "Alzheimer's." It's the most common form of dementia, so they're often right.
But when it's not Alzheimer's, there can be misunderstandings — wrong medications, or failure to recognize symptoms that can be treated. That's why it's important for health care professionals to turn over additional stones to make the right diagnosis.
A recent study suggested that a biopsy of the submandibular gland could offer similar biomarkers as found in the brain to detect Lewy body dementia early and more easily. Is there potential?
Paulson: It's an interesting study. More work needs to be done to determine whether a biopsy of the salivary gland can pinpoint the diagnosis. That study was done on biopsies of people who died from the disease. The real question is: Could we use something like that early on?
The official diagnosis of Lewy body dementia is through an autopsy. We don't do brain biopsies to make a diagnosis. We don't yet have biomarkers for the disease in the spinal fluid, which, even for Alzheimer's, is a relatively new tool. We use our clinical judgment.
How do you treat the disease?
Paulson: The treatments include cholinesterase inhibitors such as donepezil (Aricept) and rivastigmine (Exelon) … medications also used in Alzheimer's. They can help with some of the cognitive issues.
Parkinson's disease medications can improve mobility quite a bit. But it's a double-edged sword: They also can cause or worsen hallucinations. And we are reluctant to give antipsychotics or other medicines that can cause motor impairment.
How did Robin Williams' death bring attention to the disease — and dispel rumors that his suicide was solely related to depression?
Paulson: I would say that his spouse, Susan Williams, did a tremendous service to the community by getting the Lewy body name out there. People are saying, "He had what?" That made many people think about it for the first time.
Depression and dementia, unfortunately, often go hand in hand. In some cases, it's the chicken-and-the-egg question: What's causing what? We might not be certain about that.
How do Lewy body dementia support groups — through the Rinne Initiative and others — work and why are they important?
Paulson: People who are dealing with a disease like this often learn a lot from others in the same situation. There is a sharing of stories and problems, a bonding over the disease and its concerns.
Sometimes, a remarkable amount of knowledge can be transferred to someone new to the diagnosis from another family that has seen it for a while.
What is the next feasible step going forward?
Paulson: We need disease-modifying therapies and ways to slow the disease's course. Now that we know the primary protein in this disease, we have compelling ideas about ways to reduce that protein or reduce the damage it causes.
That said, we also must continue working to come up with ways to deal with that double-edged sword, treating with medication for Parkinson's symptoms without worsening psychiatric symptoms. As a doctor who treats patients, that's a major concern right now.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!