Three early-stage cancer drug projects receive pilot grants to help them advance from the bench toward the bedside.
10:40 AM
Author |

Developing new medicines is notoriously challenging and expensive — especially in cancer.
And for academic researchers, there's limited funding available to advance new ideas to the point where they're ready to compete for the large-scale federal or foundation funding needed to fully develop them.
That's why the University of Michigan invests in pilot funding for early stage drug discovery projects. Since 2012, Michigan Drug Discovery — a campuswide collaboration to find, fund and mentor projects originating from faculty research — has invested more than $2.3 million in more than 70 projects. These, in turn, have gone on to secure more than $17 million in federal grants and other support, helping them to continue advancing from the lab bench towards the bedside.
Here are the stories of three projects led by U-M Rogel Cancer Center members that were funded by Michigan Drug Discovery earlier this month.
Turning off the RNA garbage disposal
In cells, there's a protein complex called the RNA exosome that breaks down and gets rid of broken and unneeded RNA.
Cancer cells are especially reliant on a well-functioning RNA exosome because they produce an abundance of mis-spliced transcripts during their rapid proliferation, says Mats Ljungman, Ph.D., a professor of radiation oncology in the Medical School and of environmental health sciences at the School of Public Health.
"The basic idea is that if we can shut down this garbage disposal, the cancer cells will drown in their own garbage," he says.
Ljungman and collaborator Nouri Neamati, Ph.D., the John G. Searle Professor of Medicinal Chemistry at the College of Pharmacy, recently received a $70,000 grant to conduct high-throughput screening at the U-M Life Sciences Institute's Center for Chemical Genomics to find small molecules that can shut down the RNA exosome.
They previously discovered two classes of compounds that can inhibit the RNA exosome. They'll use this grant to screen for additional inhibitors that are more selective and have better properties for ultimately being developed into a drug.
The basic idea is that if we can shut down this garbage disposal, the cancer cells will drown in their own garbage.Mats Ljungman, Ph.D.
Saurabh Agarwal, Ph.D., a research scientist in the Ljungman lab, developed a process to screen for new RNA exosome inhibitors in a fast, efficient manner.
"If the enzyme works, it will degrade the substrate and we'll be able to see fluorescence," he says. "But if a compound inhibits the enzyme, it can't degrade the substrate and there's no light."
And while the prospect of a potential therapeutic target is exciting, a successful inhibitor could also help scientists learn more about how the RNA exosome functions.
"Even if we're not ultimately able to make a drug that is safe and effective in people, these compounds could still be useful reagents for studying RNA turnover and RNA biology — which would be a huge boost for the whole field," Ljungman says.
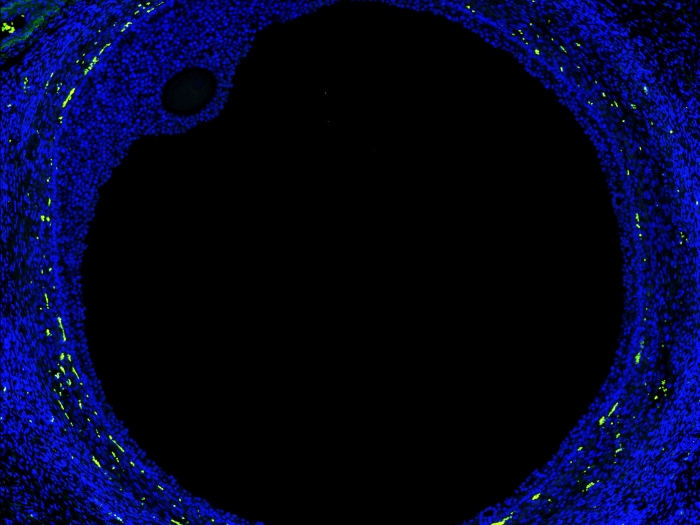
Targeting microRNA to fight ovarian cancer
The lab of Analisa DiFeo, Ph.D., studies ovarian cancer — from foundational biology to potential new biomarkers and treatments.
Unlike lung cancer, breast cancer and many other types of cancer, ovarian cancer has very few recurring point mutations — single letter typos in DNA that give rise to cancer. Instead, they have many copy number variations, where large swaths of DNA are repeated or missing, explains DiFeo, an associate professor in the Departments of Pathology, and Obstetrics and Gynecology at the Medical School.
"So that's why I started to look at microRNAs," she says. These are short fragments of RNA that bind to messenger RNA and prevent the production of certain proteins.
"In ovarian cancer, we know that we need to find a genetic driver that regulates multiple genes without needing it to be mutated," DiFeo says. "And that's the beauty of microRNA, but also the most difficult part — one micoRNA can affect 20, 30, or up to 100 different genes."
Many ovarian cancer patients respond well to cisplatin chemotherapy, but invariably their tumors grow back, and with resistance to the frontline therapy.
"So we're trying to understand the mechanisms of resistance, and what we found is that in chemo-resistant cells, a microRNA known as miR-181a is enriched," she notes.
And that's the beauty of microRNA, but also the most difficult part — one micoRNA can affect 20, 30, or up to 100 different genes.Analisa DiFeo, Ph.D.
DiFeo received a $7,500 grant from Michigan Drug Discovery for her initial work on a high-throughput screen at the Center for Chemical Genomics. The goal is to find an inhibitor that can block the action of miR-181a. The screen builds on a microRNA biosensor previously developed by the lab to monitor miR-181a function in tumor cells. If successful, she can apply for up to $75,000 for a larger screen.
Beyond ovarian cancer, data from The Cancer Genome Atlas shows miR-181a is active in other cancers and is associated with worse survival rates.
"So the hope is that if we can find a drug to target this microRNA, it won't only apply to ovarian cancer, but potentially to many other types of cancer," DiFeo says.
From microbes to immunotherapy
Amping up the body's natural immune system to find and kill cancer cells is a hot area of cancer research. Major pharmaceutical companies are competing to develop small-molecule compounds that can activate a group of proteins that induce type 1 interferons, which help regulate the immune system.
The current leading approach, however, requires the drugs to be injected directly into tumors due to off-target toxicities, and can't be used against cancers that have spread throughout the body.
So our hypothesis is that we can harness these natural systems to develop a new class of compounds that can stimulate the immune system to send out cancer-killing T cells.James Moon, Ph.D.
James Moon, Ph.D., and his co-investigators at the U-M Life Sciences Institute, are taking a different approach. They received a $75,000 grant from Michigan Drug Discovery to find candidate compounds in U-M's 40,000-sample (and growing) library of natural product extracts.
These molecules come from microorganisms that were collected from marine and soil samples across the globe. Scientists harness the chemical pathways that the organisms have evolved over millennia that help them to thrive and defend themselves. Natural products are where, for example, most antibiotics originated from.
"Our immune systems are built to recognize foreign pathogens," says Moon, the John G. Searle Associate Professor of Pharmaceutical Sciences at the College of Pharmacy, and an associate professor of biomedical engineering at the Medical School and College of Engineering. "So our hypothesis is that we can harness these natural systems to develop a new class of compounds that can stimulate the immune system to send out cancer-killing T cells."
Xiaoqi Sun, a graduate student in the Moon lab has developed a screening process and has identified more than 70 "hits" with a response comparable to or stronger than the current leading drug.
"Our goal is to identify and isolate new chemical entities that can activate our pathway of interest, verify their activation of type 1 interferons, and help us examine their efficacy in mouse models," Sun says.
U-M is uniquely positioned to make headway in this area of immunotherapy, says co-investigator Ashootosh Tripathi, Ph.D., who directs U-M's Natural Products Discovery Core.
"We have one of the world's leading libraries of natural products extracts, a state-of-the-art high-throughput screening facility and decades of experience in natural products drug discovery," he says.
The other co-investigators on the grant include: David Sherman, Ph.D., a professor at the LSI, College of Pharmacy and Medical School, and Andrew Alt, Ph.D., director of the Center for Chemical Genomics.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!