Where will the next seasonal flu virus come from? Michigan researchers look at how the virus evolves inside sick people for clues.
3:00 PM
Author |
The latest flu season may be over, but for the experts tasked with keeping the public safe from health threats, the next flu is always just around the corner.
MORE FROM THE LAB: Subscribe to our weekly newsletter
A new study by University of Michigan researchers sheds light on how the influenza virus evolves in people, knowledge that may one day enable epidemiologists to forecast just how bad a seasonal flu will be and provide more lead time for vaccine development.
When a person becomes infected with the influenza virus, the virus will copy itself inside the cells of the body. Influenza, like other RNA viruses, mutates very rapidly, says Adam Lauring, M.D., Ph.D. , assistant professor in the U-M Department of Medicine, Division of Infectious Diseases and the Department of Microbiology & Immunology. Every time it copies its genome, it's making a mistake or two. At a population level, this mutation eventually leads to the development of new strains of the flu virus and is why the composition of the flu vaccine must change every year.
To study this process, Lauring collaborated with Arnold Monto, M.D., and Emily Martin, Ph.D., MPH, of the U-M School of Public Health, using samples provided by families throughout southeastern Michigan. The samples are collected as part of a Centers for Disease Control and Prevention-funded program that monitors the spread of seasonal flu throughout the U.S. and the effectiveness of the flu vaccine.
When members of the participating families get sick, they are asked to take swabs from their noses and throats, put them in a vial and take them to Monto's lab. The researchers can then test the samples to determine which virus that person has. They also collect other epidemiologic information, such as the person's age and whether they were vaccinated or have flu antibodies.
For their work, published in the online journal eLife, Lauring and his graduate student JT McCrone used the same samples to study the viruses themselves.
"It's often hard to study disease transmission in the real world. These samples are valuable because they come from a population where people are getting naturally infected with the flu and transmitting it to each other," Lauring says.
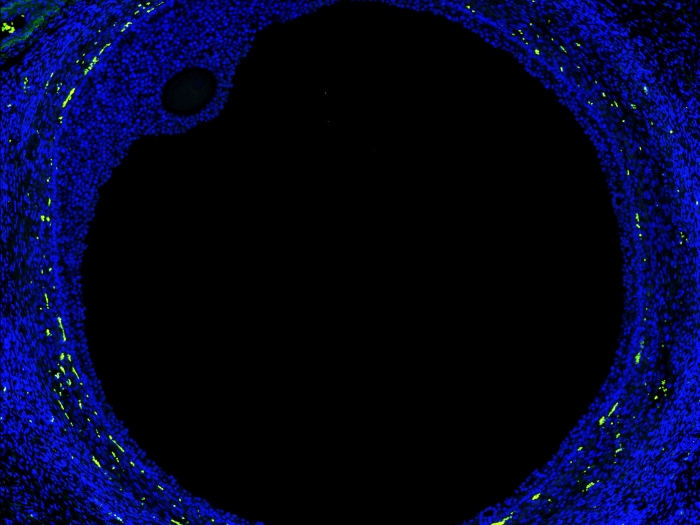
Using samples from about 50 people who submitted two swabs over the course of several days, Lauring's lab harnessed next-generation sequencing technology provided by the University's Biomedical Research Core Facilities to sequence each virus's genome an average of 10,000 times. From the resulting data, they determined the most common virus sequences each person had, and they found rarer mutations in some of the viruses.
If you have a 100 million people infected in the world, even a random and inefficient process will happen with some frequency.Adam Lauring, M.D., Ph.D.
Selecting a new flu virus
During seasonal flu outbreaks, the virus will spread throughout an area until enough people get infected and develop antibodies against it to prevent its further transmission. Of course, another way to reduce the spread of flu is by getting a flu shot. Herd immunity develops when enough people are vaccinated or previously exposed, limiting the flu's ability to spread.
SEE ALSO: How a Virus Tricks Cells into Helping It Build an Invasion Route
But new flu infections can emerge when a virus has mutated enough to evade this immunity. This is how flu evolution works at the population level. What Lauring and his colleagues wanted to know is how the influenza virus evolves within individuals and whether the virus was changing to avoid a given person's immune system.
What they discovered is that most mutations to the flu virus within a person rise and fall somewhat randomly. "Our data is telling us that that process of selecting a new virus is inefficient. It doesn't work very quickly and certainly not quick enough to happen over the four or five days that someone has the flu."
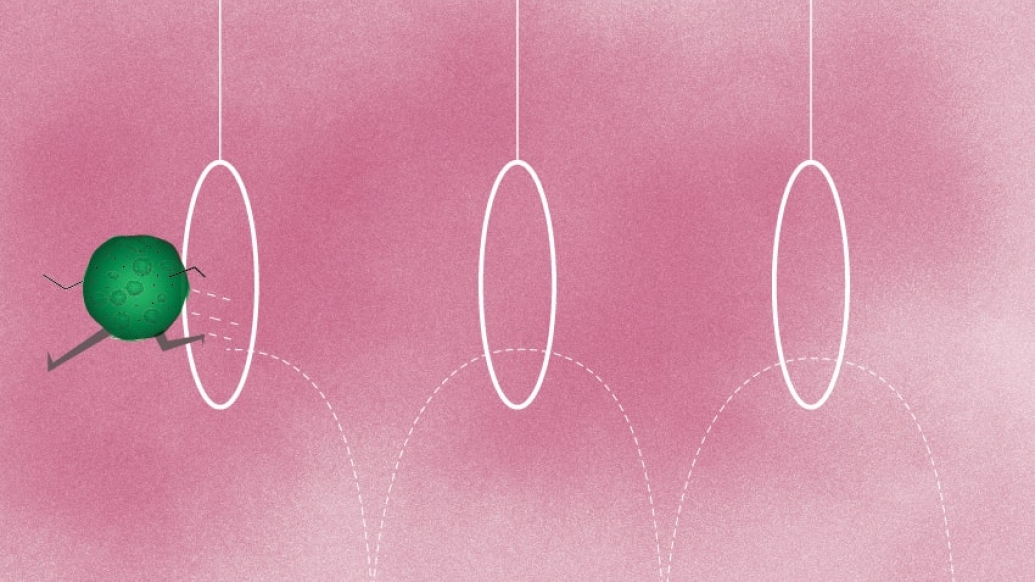
The research team was also able to compare viruses from members in the same household to see which ones were being transmitted. By comparing one person's virus mixture to another's, they found that only one or two viruses — from a collection of hundreds or thousands — are transmitted.
This means influenza evolution is "a very inefficient process, and a lot of these viruses that are developing in a person are really not going anywhere," Lauring says. But new influenza viruses have to come from somewhere, Lauring says, adding, "If you have a 100 million people infected in the world, even a random and inefficient process will happen with some frequency."
He hopes future research on how the flu evolves in communities might allow scientists to more quickly pinpoint exactly when and how this happens — and protect more people from illness.
Lauring's study was funded by the National Institutes of Health and the Doris Duke Charitable Foundation. Monto's study was funded by the Centers for Disease Control and Prevention and the National Institutes of Health.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!