Every year, 1 in 1,000 people with epilepsy dies suddenly. Scientists are using stem cells from children with rare seizure disorders to find answers and potentially guide treatment.
7:00 AM
Author |

Every second of every day, trillions of cells in our body let in tiny atoms of sodium — like dogs or cats passing through a pet door on a house.
MORE FROM THE LAB: Subscribe to our weekly newsletter
This constant traffic through what scientists call "sodium channels" helps our cells talk to one another, send information along, and respond to outside threats.
But on rare occasions, this flow goes terribly, lethally wrong. And when it does, a child who kissed her mother good night just hours before never wakes up. Or a young adult goes into a seizure that only stops when his heart does.
One out of every 1,000 people with epilepsy or other seizure disorders dies each year in this way — a phenomenon called sudden unexpected death in epilepsy, or SUDEP. For those who don't have their seizures under control through medication or other means, and for those with certain genetic syndromes, the risk is much higher.
New scientific research aims to reduce that risk by understanding why it exists in the first place.
Much of the work focuses on the brain and the heart, because SUDEP appears to stem from a simultaneous haywire reaction deep in the tissues of both organs. Sodium channels, researchers say, appear to play a key role.
Lori Isom, Ph.D., didn't start out studying sodium channels to try to solve SUDEP. But after meeting families who have lost children to it, or who live in fear that they will, her team's work now centers on this goal.
"In patients who have thousands of seizures in their lives, we need to understand why they experience the one that kills, and what perfect alignment of the planets has to happen in their brains and hearts," says Isom, who chairs the department of pharmacology at the University of Michigan.
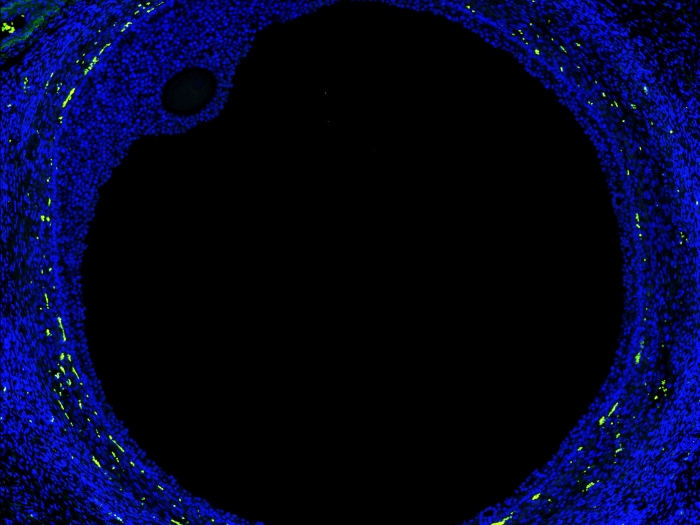
She and other scientists at U-M Medical School are looking for clues to SUDEP using mice that have been genetically engineered to express human epilepsy mutations. They are also using skin cells from the most seizure-prone patients to produce stem cells that can be grown in the lab.
From these stem cells, they can carefully grow heart and brain cells, and study how their development and activity differ from that of cells grown from non-seizure-prone people.
In patients who have thousands of seizures in their lives, we need to understand why they experience the one that kills, and what perfect alignment of the planets has to happen in their brains and hearts.Lori Isom, Ph.D.
Forecasting a 'perfect storm'
In a paper in the latest issue of the Proceedings of the National Academy of Sciences, Isom, Miriam Meisler, Ph.D., and their colleagues report on highly unusual activity in heart cells that contain a key mutation in a gene that cells use to build sodium channels.
Meisler, a professor of human genetics at U-M, helped pioneer the techniques that allow mice to mimic human disease so they can be used as a model for real patients.
The cells were isolated from the hearts of mice that express a genetic mutation discovered in a patient who was born with an especially risky condition known as early infantile epileptic encephalopathy (EIEE). One in 10 children with this condition will die of SUDEP.
In EIEE, a mutated gene known as SCN8A causes cells to make a faulty form of the sodium channel called Nav1.6. And the mouse heart cells the scientists tested showed the effect of that mutation: hyperexcitable cells that contracted abnormally in patterns that would cause irregular heartbeats if they were inside a human heart.
The mice carrying this genetic defect had reduced heart rates. When given adrenalin or caffeine, their hearts went into dangerous abnormal rhythm patterns known as ventricular arrhythmias.
The findings, then, support the argument that SUDEP arises from a kind of "perfect storm" of misfiring brain and heart cell activity.
Isom, Meisler, and their colleague, Jack Parent, M.D., previously reported on the effects of another sodium channel mutation, in the gene SCN1A. That work was done in brain cells grown from patients with Dravet syndrome, another often deadly seizure disorder that arises in children in their first year of life.
But more recent work by a European team that studied the SCN1A mutation in mice only deepens the mystery of what's going on, Isom and a colleague comment in a new piece in Epilepsy Currents.
"In addition to causing seizures, these mutations create a substrate for heart rhythms that can threaten a life," says Isom, who now serves with Parent and Meisler on the Dravet Syndrome Foundation scientific advisory board. "What all this means is that, especially in kids with these genetic seizure disorders, we need to be looking closely at their hearts as well as their brain."

More work ahead
While the new scientific results can't tell doctors what to do for patients who have epilepsy — or more dangerous rare genetic seizure disorders — Isom, Meisler and Parent have begun to field questions from parents of at-risk kids, teens and young adults.
More detailed testing of nerve-firing patterns, using heart and brain tests such as electrocardiogram and electroencephalogram may prove useful in such patients when a seizure sends them to the hospital. Longer-term monitoring of heart rhythm, using a wearable device called a Holter monitor that's typically used for people with a diagnosed heart arrhythmia, may also be considered.
SEE ALSO: Improving Access to Care for Children with Epilepsy in Michigan
Meanwhile, families with genetic seizure disorders have flocked to the U-M investigators with offers to allow their children to donate tissue samples so that scientists can spell out the exact nature of their genetic defect and study its impact in skin cell-derived stem cells. The Dravet Foundation offers such families more information about taking part in research.
By tracking such donors over the long term, researchers hope to eventually discover biomarkers for SUDEP — something detectable in the blood or tissue that could predict how much of a risk of sudden death a seizure patient faces.
Isom and Parent are working with teams at 13 other institutions on a SUDEP "center without walls" funded by the National Institutes of Health to do just that.
Other scientists are looking at how the body's control of breathing, or its ability to rouse a person out of sleep, might change in SUDEP-prone people, for instance.
The ongoing pursuit has been highly personal.
"The chance that we have had to know the patients and families, and to know that they are waiting for the outcome of our research, has completely changed our thoughts about our work, and the experience of those who are training in our labs," says Isom. "The link to the patient gives it added urgency — the feeling that we're doing this because someone really needs it."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!