U-M researchers are investigating a new immunotherapy drug for AML in children — one with a built-in "safety switch" in case unexpected adverse reactions occur.
7:00 AM
Author |

In the search for childhood cancer cures, most headlines focus on finding effective treatments.
SEE ALSO: Doctors Unleash New Weapon to Fight Pediatric Neuroblastoma
It's understandable, after all. Saving lives is the ultimate goal.
But an equally challenging and important question is whether potential therapies will cause harm.
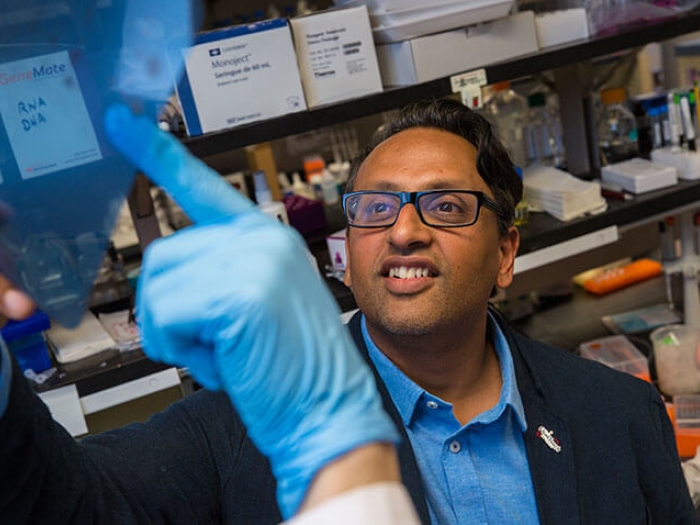
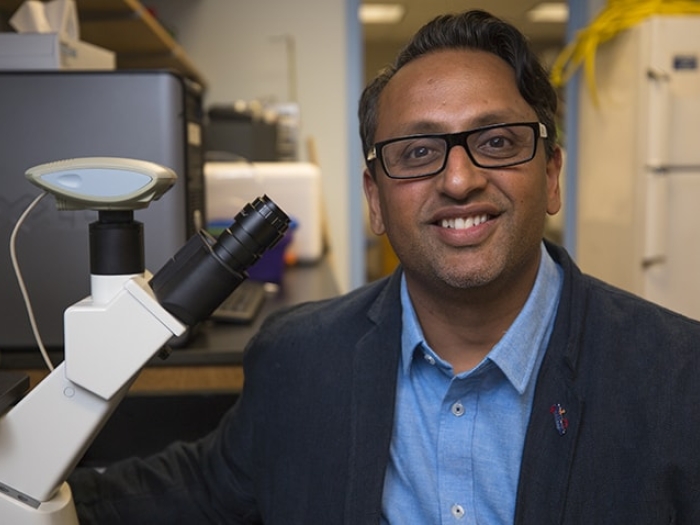
"The field of oncology research is about finding better and safer cures," says Challice Bonifant, M.D., Ph.D., pediatric oncologist at University of Michigan C.S. Mott Children's Hospital.
Benefits versus potential harm
U-M is home to the largest portfolio of clinical trials for children with relapsed or refractory cancers in Michigan. For these high-risk patients, the same side effects considered unsafe for a patient with a new, uncomplicated cancer may be considered worth the potential toxicity because of the severity of the condition.
"When a patient fails standard treatment protocols and we move into experimental therapies, we have to evaluate the safety of a drug through a different filter," says Bonifant.
Bonifant is among a cadre of new cancer warriors focusing on how to make new, emerging cancer therapies safer for children.
Her work focuses on treatments for acute myeloid leukemia (AML), a blood cancer that needs new therapies, as children with the high-risk disease have little chance of cure.
For these patients, simply using traditional drugs in higher concentrations won't work. They encounter life-threatening complications and severe toxicities.
"It's not just about limiting inconvenient side effects. In my work, for example, we're focusing on how to manage powerful emerging treatments so we can use them more effectively," Bonifant says.
There is no doubt in my mind that these therapies are part of the future for children fighting cancer. But we have to make them safe before we can let them do their job.Challice Bonifant, M.D., Ph.D.
Emerging treatment areas for AML
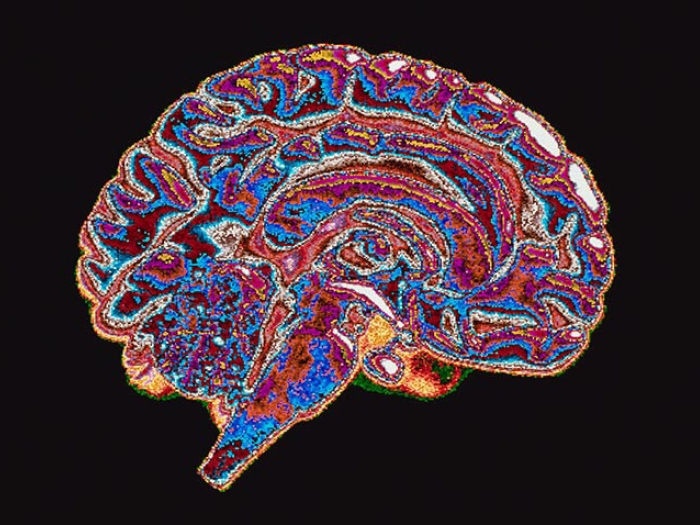
One of the most promising emerging treatment areas for children with AML is a new class of therapies called immunotherapy. Immunotherapy uses the body's own immune system to more efficiently attack cancer cells.
Infusion of a type of immune cell, the T cell, modified to specifically recognize a cancer cell has been successful in early pediatric acute lymphoblastic leukemia (ALL) studies. A similar approach could work with AML.
"Based on what we've seen with ALL, we have developed a new type of modified T cell, genetically engineered to secrete a targeting engager molecule that directs these cells, as well as unmodified T cells, to attack AML cells," says Bonifant.
Preliminary studies have shown strong activity against AML in a preclinical animal model that mimics human disease.
"The drugs can only do their job, though, if we can find ways to control them and limit their toxicity so that we can continue treatment long enough to effectively kill the cancer," says Bonifant.
Bonifant's current research is exploring how to initiate a "safety switch," which will allow rapid destruction of AML-specific T cells if unexpected toxicity is seen.
The key to triggering the safety switch is a signal Bonifant and her team introduced onto the T cell surface that can be recognized by an FDA-approved antibody, rituximab. So far, lab results are promising.
"Our preliminary research has found not only that the safety signal does not limit the drug's effectiveness against AML, but that activating the switch results in elimination of the modified cells," she says.
"We hope further research will prove that if unexpected toxicity resulting from our developed T-cell therapy does occur, we turn the safety switch on, to turn the toxic T cells off."
The next steps
Progress can't come fast enough for families of kids diagnosed with AML.
SEE ALSO: How Very Aggressive Cancer Cells Use Energy to Grow
"We're currently in the preclinical portion of our research, testing the safety-switch mechanism in animal models. Our next step is to develop a clinical trial with a goal of ultimately benefiting patients with AML," she says.
Grants from Alex's Lemonade Stand and the WES Leukemia Research Foundation partially funded Bonifant's earlier work. This week, the Hyundai Hope on Wheels Foundation awarded her lab an additional $250,000 grant to continue her research. With the additional funding, the laboratory will initiate investigation into combining "checkpoint blockade" with T-cell therapy, to make the activated T cells stronger and more powerful.
"There is no doubt in my mind that these therapies are part of the future for children fighting cancer," says Bonifant. "But we have to make them safe before we can let them do their job."
This post is part of a series of articles on breakthrough pediatric cancer research during Childhood Cancer Awareness Month. Learn more about how you can play a role in the fight to #BlockOutCancer.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!