Patients prescribed benzodiazepines and opioids by different providers 20% more likely to overdose, adding to already heightened risk.
2:05 PM
Author |
For years, experts have warned of the risks of combining certain sedatives and prescription pain medications – for instance, Xanax and Vicodin, Valium and Norco, or Restoril and Percocet. Now, a new study shows that this combination is especially risky if multiple doctors prescribe the two different types of drugs to the same patient rather than the same doctor.
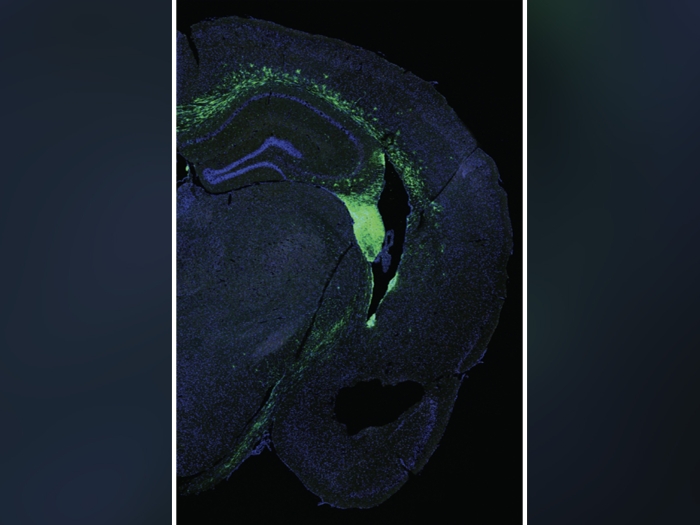
The two classes of drugs, called benzodiazepines and opioids, both act on the brain. Benzodiazepines are prescribed for anxiety, insomnia, and panic attacks, while opioids are prescribed for pain. Because both suppress the drive to breathe, past studies have shown a higher risk of overdose among patients who take opioids and benzodiazepines at the same time.
The new study shows that the risk of overdose is even higher for patients who filled current prescriptions for both drugs, but whose prescription were written by two different providers. After adjusting for differences in patient characteristics and prescription dosing, the risk was 20% greater.
The finding comes from an analysis of private insurance and Medicare Advantage claims among more than 529,000 people over the age of 12 who had overlapping benzodiazepine and opioid prescriptions between late 2016 and the end of 2018. It's published in JAMA Network Open by a team from Michigan Medicine, the University of Michigan's academic medical center.
"We know that having overlapping opioid and benzodiazepine prescriptions is one of the strongest risk factors for overdose. Our findings suggest that the circumstances that lead to these overlapping prescriptions matter. For example, if a psychiatrist prescribes a benzodiazepine to a patient whose primary care doctor is already prescribing opioids, that may be more dangerous than if the primary care doctor writes both prescriptions," said Kao-Ping Chua, M.D., Ph.D., lead author of the new study.
Chua notes that the reasons for the increased risk aren't clear, but he speculates that it involves lack of coordination, a known risk factor for overdose. "Because of differing health record software, a doctor in one system might prescribe a benzodiazepine without being aware that the patient is being prescribed an opioid by a doctor in another system. This results in missed opportunities to co-prescribe naloxone and educate patients about the risk of overlapping opioid and benzodiazepine prescriptions," he said.
Chua notes that one solution would be to create an alert to co-prescribe naloxone in electronic health records anytime a doctor tries to prescribe an opioid to a patient who is prescribed a benzodiazepine by another doctor in the same system. He also notes that many states require prescribers to check a Prescription Drug Monitoring Program before prescribing controlled substances, which allows them to see if their patient is taking a medication that could clash with the one they're prescribing.
However, Chua notes that these high-tech solutions would not be needed if doctors did a better job of taking a complete medical history. This includes a list of all medications patients are taking.
Overall, 44% of patients only had overlapping prescriptions from one prescriber and 28% only had overlapping prescriptions from multiple prescribers. Nearly 38% of the days of overlap between opioids and benzodiazepines involved prescriptions from multiple prescribers.
Overall, 1 in 231 patients had an overdose during a period of overlapping opioid and benzodiazepine prescriptions. Chua notes that this proportion would be even higher if the study had counted overdoses that resulted from leftover medications that weren't taken during this period.
Paper cited/DOI: JAMA Network Open. DOI:10.1001/jamanetworkopen.2021.20353

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!