Tests to diagnose or monitor aren’t without risks, suggesting a need for further research, physician training and frank doctor-patient conversations.
7:00 AM
Author |
A recent Neurology study examining two patient cohorts of similar age and ailments revealed a stark diagnostic difference.
Medicare recipients were more than twice as likely to receive "potentially inappropriate" imaging for headaches than those who reported the same symptoms at Department of Veterans Affairs health care facilities, the study found.
MORE FROM THE LAB: Subscribe to our weekly newsletter
Among neuropathy cases from the same two outpatient groups, both comprised of individuals ages 65 and older, the imaging rate for patients with Medicare was almost three times greater.
Such disparity speaks to a larger debate.
Under which circumstances is a screening — a scan, a blood draw, a biopsy — necessary? Why do procedural divides exist? And when might these procedures cause more harm than good?
As medical technologies become increasingly precise, roadblocks lurk among the gains: Over-imaging in low-risk populations can detect benign abnormalities, return false positives, heighten a patient's anxiety and waste money.
With headaches, "you image 100 people and are lucky if you find a brain tumor in one," says James Burke, M.D., a neurologist at the University of Michigan Health System, a member of the Institute for Healthcare Policy and Innovation and a co-author of the Neurology study. "For migraines, you should almost never image."
Still, he says, nearly half of patients with headaches eventually get an MRI — pre-emptive action fueled by "a culture where we like to feel reassured" and fear of malpractice claims if a problem is missed.
On the other hand, scans that reveal incidental or slow-growing discoveries could prompt avoidable or even hazardous surgery. A person might also be exposed to needless radiation and, if further steps aren't taken, suffer unwarranted panic.
Many practitioners acknowledge the Catch-22 — one that in 2009 totaled $210 billion worth of unnecessary services, according to a report from the Institute of Medicine.
"It doesn't take long as a physician to realize we do a lot of testing that doesn't help people," says Brian Callaghan, M.D., a UMHS neurologist, an IHPI member and a co-author of the Neurology report.
His research has helped foster screening guidelines for Choosing Wisely, an American Board of Internal Medicine Foundation initiative launched in 2012 to help clinicians decide when — and when not — to issue tests (similar resources are available for patients).
Nine medical societies provided input upon founding. Choosing Wisely now uses recommendations from 75 groups, including the American Academy of Neurology and the American College of Radiology.
The growth seemingly reflects an industry shift.
"A decade ago, nobody was having these conversations. Now, the pendulum has swung," Callaghan says.

Rethinking the approach
With this dialogue comes a deeper review on who may benefit most from certain tests — with age, race, lifestyle and family history playing a greater role in the decision, depending on the illness (or potential of one) at hand.
SEE ALSO: When It's Not Exactly Cancer: Renaming Early Stage Thyroid Tumors
A data-driven approach could help doctors order tests more thoughtfully and reduce negative outcomes. At the same time, it can lead to more uniform practice among facilities.
What can't be discounted in deciding whether to screen, however, is the human element: patients with recurring pain, unsuccessful treatment regimens or noticeable reason to proceed.
"The most important thing you look at is the patient in front of you," says Jennifer Griggs, M.D., M.P.H., a UMHS oncologist with a clinical specialty in breast cancer, also an IHPI member. "But if the patient has no symptoms, it's important to follow evidence-based guidelines."
Which explains why the push to target and minimize over-imaging has become a greater focus in medical research.
Among recent developments:
-
A 2016 U-M study, co-authored by Griggs, which determined nearly two-thirds of women with early stage breast cancer received unnecessary advanced imaging (via CT, PET or bone scans) to look for metastases — which are found in only 1 percent of patients. On the other hand, "upstaging" to metastatic disease could alter the course of treatment in that small group of patients, illustrating the complexity involved.
-
The discovery that an increase in post-treatment imaging of thyroid cancer patients did not always improve survival rates. The June 2016 study, culled from a database of 28,220 cases, found that such imaging was associated with more diagnoses of reoccurrence but not with, in most instances, a change in mortality. "There's some sort of line we have to draw in terms of what imaging is appropriate and not appropriate," says Megan Haymart, M.D., an endocrinologist at the University of Michigan Medical School, IHPI member and the study's senior author.
-
Controversy over a recent Northwestern University report linking "skyrocketing" rates of metastatic prostate cancer to a 2012 U.S. Preventive Services Task Force recommendation to discontinue prostate-specific antigen (PSA) testing in all men. Although the Northwestern methodology was heavily criticized, the conversation over which men should get PSA screenings continues.
-
A continued push to curb imaging as a first line of offense for chronic conditions, such as lower back pain. Odds of discovering an unrelated abnormality in the process, U-M's Callaghan says, are greater than 50 percent and often lead to drastic steps without additional review. "We do way too many back surgeries probably initiated by the diagnostic cascade," he says.
Even when appropriate, conveying the message of long-term awareness versus immediate action can be difficult for a patient to comprehend.
"It's hard not to do something," says Callaghan, "even when the best answer is to do nothing."
It's hard not to do something, even when the best answer is to do nothing.Brian Callaghan, M.D.
Balancing benefit and risk for patients
Since CT scans were introduced in the 1970s, the capacity to scrutinize the human body for signs of trouble has never been better — aptitude that also harbors consequence.
SEE ALSO: For Breast Cancer, When Does Worry Outweigh Risk?
"We now can get amazing, clear pictures of what the anatomy looks like. It's so intrinsically compelling, it makes everyone feel better to say we looked and there's nothing there," says Burke, the UMHS neurologist.
"But as we get experience with this technology, we see it's very, very common that we find something. Even though the 'something' is overwhelmingly likely to be insignificant, we often feel the need to act in response."
Which makes the concept of "watchful waiting," or active surveillance, all the more applicable.
Because imaging can now display the thyroid area in great detail, physicians might opt to monitor a tiny nodule — something they couldn't feel with their hands — rather than take the invasive step of removing it, for example. Or keep tabs on a small, slow-growing prostate cancer instead of performing a prostatectomy that could leave a man incontinent or impotent.
Such restraint might seem to conflict with the inherent duty of medicine.
"When someone gets a diagnosis of cancer, it's life-changing — everyone wants to walk away [after treatment] and say: 'I'm cured,'" says Haymart, the U-M professor researching thyroid cancer follow-up screenings.
"[But] it's important to fine-tune the treatment and the surveillance to the severity of the disease," she says. "There's a lot of room for improvement."
A need for doctor-patient conversations
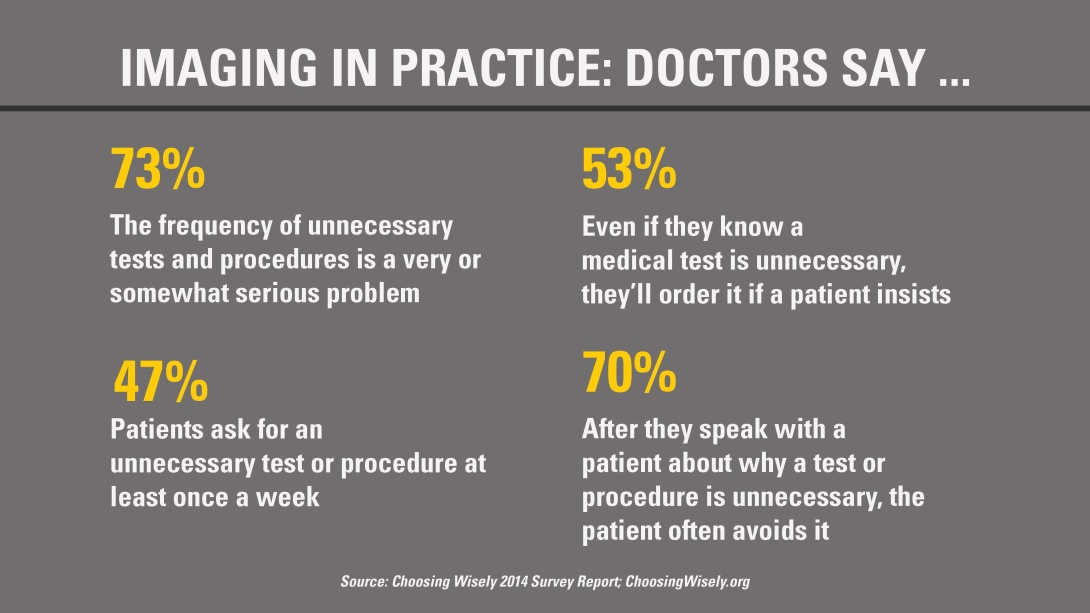
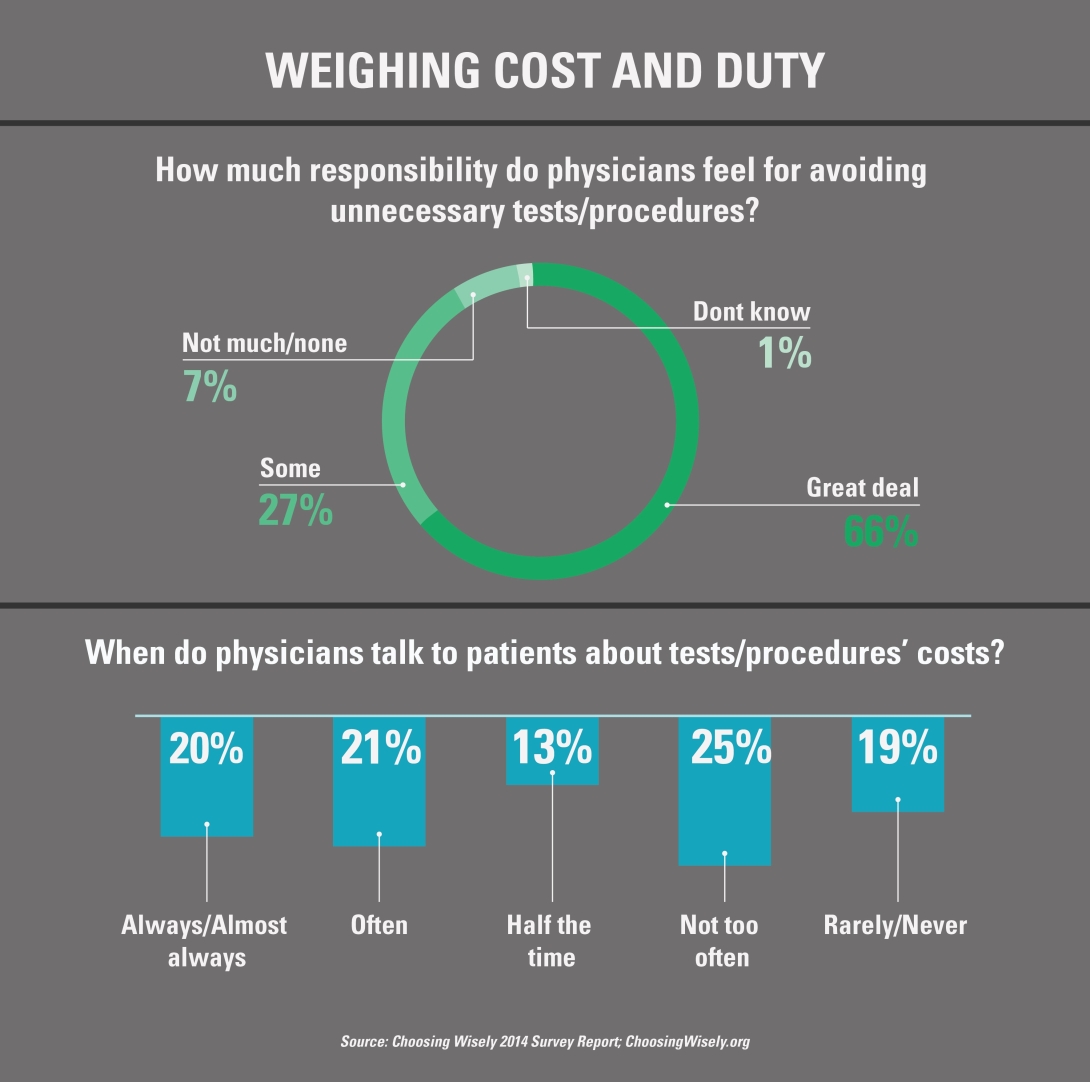
Beyond better training doctors to order imaging only when appropriate, and more research on imaging and testing's risks and downsides, added weight might be placed on patients' attitudes and preferences.
In other words, how much does a patient want to know if a minor or unexpected abnormality is detected?
Bodies, after all, aren't perfect.
Nor is the answer, says Kayte Spector-Bagdady, J.D., M.Bioethics, a postdoctoral research fellow at the Center for Bioethics and Social Sciences in Medicine at the University of Michigan Medical School and an IHPI member.
"The problem is, there's been an underestimation of the cost of giving patients too much information," says Spector-Bagdady, who co-authored a June 2016 paper in the Journal of the American College of Radiology that examined the challenges for physicians in disclosing secondary or incidental findings. "Doctors are generally so concerned about the potential harm of not disclosing information that they often don't spend enough time thinking about the potential harm of the disclosure itself."
Nonetheless, a balanced discussion before ordering a test can allow doctors to offer perspective.
This often helps a patient rationalize the situation at hand — something that can't be achieved after a screening has already taken place, Callaghan says.
Still, he adds: "I don't think those conversations happen nearly enough."
Doctors ought to take every opportunity for discussion, says Griggs, the UMHS oncologist. She also encourages patients to do their own research (within reason) and come to their appointments with questions.
This can help ensure that screenings and any resulting action are done only when in a patient's best interest.
"If it's a habit to order the test, changing the habit can be hard," Griggs says.
Callaghan, meanwhile, wants to see further research and better identification of overused screenings to help doctors better understand their low-yield value.
That will help shift such perspective into practice, even if the alternative requires some added detective work.
Burke says, "We have to ask: What is the real goal here, and are there ways of achieving that goal that don't necessarily involve getting that extra test — or a simple alternative without the same degree of downside?"
"It's hard to make intelligent judgments about weighing small risks against small benefits, but by no means is it a given that more is more."
The following disclosures have been reported: Brian Callaghan, M.D.; Impeto, Advance Medical, Kaiser Permanente, American Academy of Neurology. James Burke, M.D.; National Quality Forum, University of California-San Francisco. Jennifer Griggs, M.D., MPH; Cleveland Clinic Foundation. Kayte Spector-Bagdady, J.D., M.Bioethics; International Association of Clinical Research Nurses, Project HOPE: The People-to-People Health Foundation, Inc., University of Virginia, Duke University.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





