A survey and interviews with newly covered Michigan residents show a positive effect on physical and mental health — and, in turn, employment.
10:20 AM
Author |
Most low-income Michigan residents who signed up for the state's expanded Medicaid program say their new health insurance helped them do a better job at work, or made it easier for them to seek a new or better job, in the first year after they enrolled, according to a new study.
MORE FROM THE LAB: Subscribe to our weekly newsletter
That's on top of the positive health effects that many said their new coverage brought them, University of Michigan researchers reported at the annual research meeting of the AcademyHealth research organization.
Of the 4,090 people surveyed for the study, 80 percent had incomes below the federal poverty level, and 28 percent were out of work. All were covered by the Healthy Michigan Plan, Michigan's Medicaid expansion program under the Affordable Care Act.
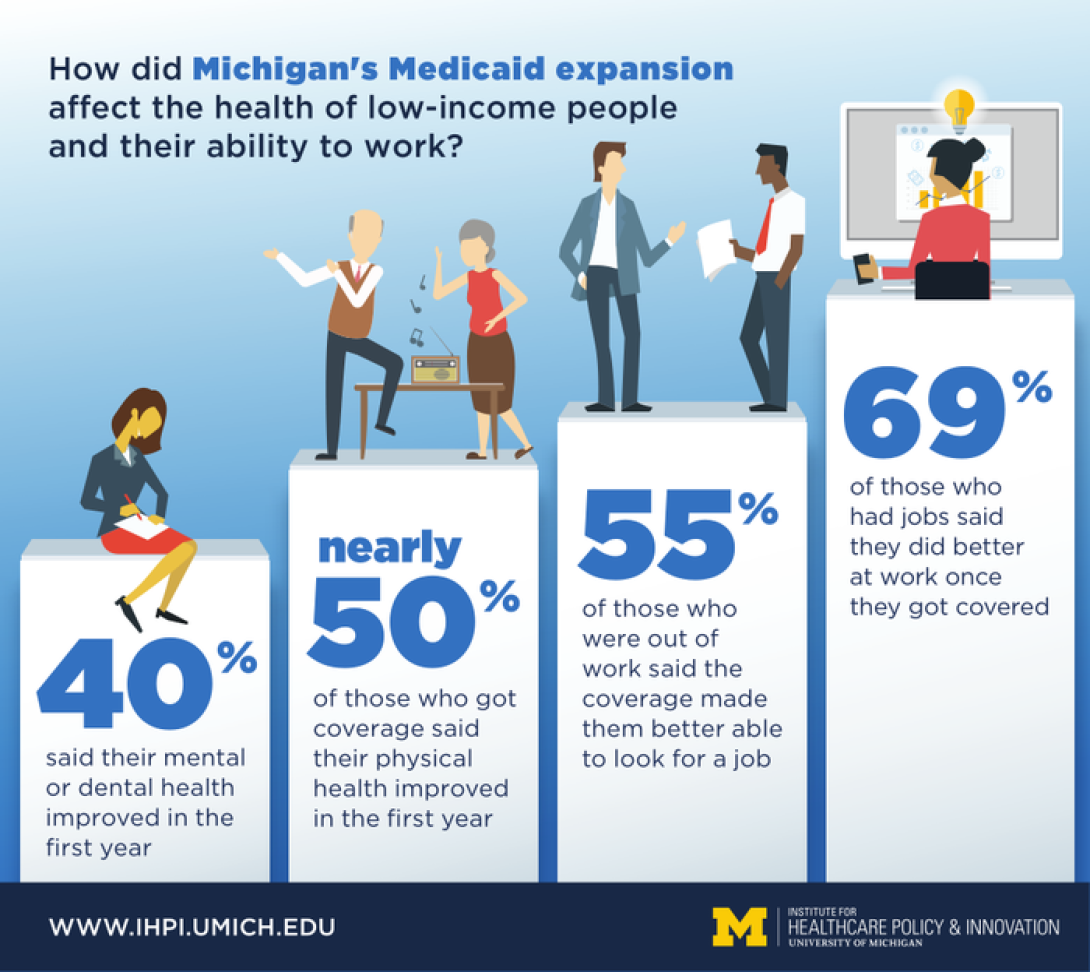
In all, 69 percent of those who had jobs said they did better at work once they had health insurance. And 55 percent of those who were out of work said the coverage made them better able to look for a job.
Having health insurance, and being able to take care of one's health as a result, has a large positive impact on a person's ability to do a better job at work or seek employment.Renuka Tipirneni, M.D., M.Sc.
Better health through coverage
Nearly half of all respondents said their physical health improved in the first year of coverage, and nearly 40 percent said their mental or dental health did.
Those who reported health improvement were most likely to experience an effect on their work life. As a group, they were four times more likely to say Medicaid coverage helped them at work. And those who felt their health had improved, but were out of work, were three times as likely to say that their coverage helped them look for a job.
"Having health insurance, and being able to take care of one's health as a result, has a large positive impact on a person's ability to do a better job at work or seek employment," lead researcher Renuka Tipirneni, M.D., M.Sc., says. "Given that a large portion of those with chronic illness or poor health are already working, this has many implications for the way we structure Medicaid programs."
She says she and her colleagues at the U-M Institute for Healthcare Policy and Innovation were surprised at how many reported better health after a short period of coverage. Studies in other expansion states have not shown overall improvement so soon.
But the impact on employment was even more surprising, she says, and applies to current debates over state and federal public policy, including proposals to require Medicaid enrollees to work or actively seek work.
Study methodology
In 2015 and 2016, Tipirneni and colleagues surveyed a representative sample of Healthy Michigan Plan enrollees, and conducted structured interviews with 67 participants, as part of a federally mandated evaluation of the program. They communicated with participants in their choice of English, Spanish or Arabic.
SEE ALSO: Medicaid Expansion More Than Pays for Itself, Study Finds
IHPI contracts with the Michigan Department of Health and Human Services to carry out that evaluation, and the new data are also described in a report on the website of the federal Medicare/Medicaid agency. In all, 672,576 Michigan residents are covered by the plan.
At the AcademyHealth meeting, Tipirneni laid out the findings of the survey, including new data about what Healthy Michigan plan enrollees say about their own health.
Impact of coverage on work
Working-class Michiganders with chronic health conditions made up more than two-thirds of all those surveyed and nearly half of those who were working. They reported a significant increase in their ability to do a good job at work in their first year of coverage.
One-third of the participants who said they were in fair or poor health held down jobs. A slightly smaller percentage of this group was out of work.
"Our findings show that many people in the Healthy Michigan Plan who aren't healthy overall are working nonetheless, and so are many people with chronic conditions," says Tipirneni. "We intend to study these participants in future work, to understand what factors influence their ability to hold or seek employment."
The remaining third of those who said their health was fair or poor said they weren't working because illness, disability or other issues made them unable to. The researchers did not ask about caregiving responsibilities that might have accounted for some people's inability to work.
The in-depth interviews with selected participants revealed personal stories behind the numbers. For instance, they described how receiving mental health care had made them more able to work, or how dental work allowed them to feel more professional while job searching.
The Healthy Michigan Plan coverage is open to any Michigan resident making less than 133 percent of the federal poverty level. Individuals working a full-time job at Michigan's 2016 minimum wage of $8.50 per hour would make just over that threshold if they lived alone, but would be eligible if they support a child or another adult who doesn't or can't work.
The U-M team is also presenting other findings about Michigan's Medicaid expansion in research posters at the AcademyHealth meeting, including:
-
Survey results and structured interview results suggesting that Healthy Michigan Plan enrollees reduced their reliance on urgent care clinics and emergency departments, and increased their use of primary care, after enrolling
-
Data showing that enrollees who had mental health or substance use issues had better access to care and better mental health after enrolling
-
Findings about the impact of the Michigan plan's dental care provisions, showing that it improved the health of their teeth and gums but that many enrollees were not aware of the benefit
-
An evaluation of the early impact of the Michigan plan's cost-sharing features, which were intended to encourage enrollees to be cost-conscious about their care
-
An exploration of the program's impact on enrollees who have chronic health conditions, or were found to have them after seeking medical care with their new coverage
-
A report on how low-income Michiganders would want to allocate coverage if they were designing a plan for people like themselves, given a set amount of resources, including the cost and access trade-offs they would be willing to make
More information about the ongoing Healthy Michigan Plan evaluation and other Medicaid-related research from IHPI members is available at IHPI.UMich.edu.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!