Traditional Medicare spends much more on post-hospital care for people in their 60s than private insurance, but the additional spending doesn’t keep patients from ending up back in the hospital.
2:14 PM
Author |

Picture a woman in her 60s, in the hospital, after a heart attack or hip replacement. As her hospital stay nears its end, her care team prepares her for the next step in her recovery, which might include time in a nursing home or rehabilitation facility, care at home or regular therapy appointments.
But a new study reveals that if the patient has traditional Medicare coverage, her post-hospital care will probably cost far more than it would have for an identical patient with private insurance.
And despite the difference in cost, both patients have about the same clinical ending – as measured in their odds of being readmitted to the hospital, the study shows.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily updates on iTunes, Google Play and Stitcher.
The new findings, made by a University of Michigan team, suggest that the Medicare system spends far more than it probably needs to on post-hospital care. That spending is about $60 billion a year.
The researchers say that changes to Medicare's post-hospital care payment structure, to bring it closer to that used by private insurance, might save taxpayer dollars while still giving patients the care they need to recover and avoid a repeat hospital stay.
As elected officials and presidential candidates put forth proposals to expand Medicare, this new study also offers insight into a major source of potential cost if any of those proposals become law. It also shows the importance of developing guidelines to help clinicians choose appropriate post-hospital options for each patient.
This shows that providers are making similar clinical decisions about what to do regarding post-hospital care for both types of patients, but that Medicare is far more permissive regarding the volume of services delivered and therefore the costs.Scott Regenbogen, M.D., M.P.H.
Comparing costs
The new analysis, published in the September issue of Health Affairs, used four years' worth of data from more than 25,000 patients across Michigan whose hospitals take part in a statewide effort called the Michigan Value Collaborative.
Funded by Blue Cross Blue Shield of Michigan, MVC pools data from patients who have different forms of insurance and finds ways to improve quality and value.
The new study, funded by the National Institutes of Health's National Institute on Aging, focuses on MVC data from people in their 60s. It included people below and above age 65, the age of Medicare eligibility, who have either traditional Medicare coverage or BCBSM plans called PPOs, which cover about 20% of all Michigan residents.
The researchers used statistical techniques that allowed them to make 'apples to apples' comparisons of post-hospital care use and costs between the two groups.
The study focused on the use and the cost of post-hospital care received at home, in skilled nursing facilities and at inpatient and outpatient rehabilitation facilities. It included those hospitalized for six common reasons: heart attack, heart failure, cardiac bypass surgery, stroke, hip replacement and colon surgery.
For almost every condition and every form of post-hospital care, there was significantly more spending for Medicare patients than privately insured patients. Post-hospital spending was more than double for hip replacement patients covered by Medicare than for privately insured patients. It was two-thirds more for Medicare participants who had had heart bypass surgery.
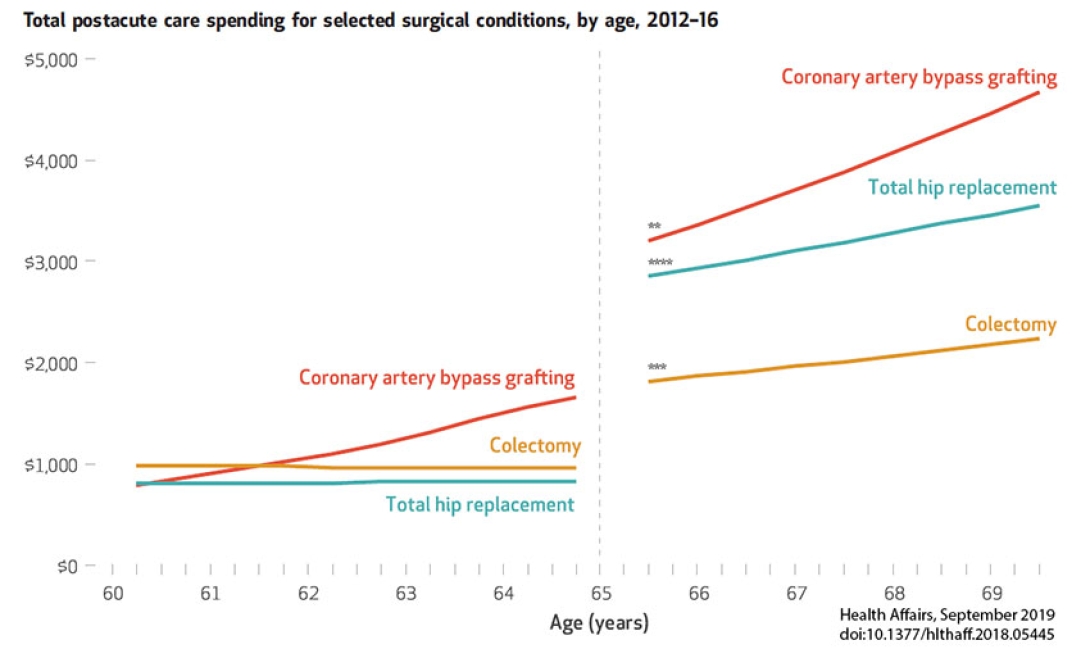
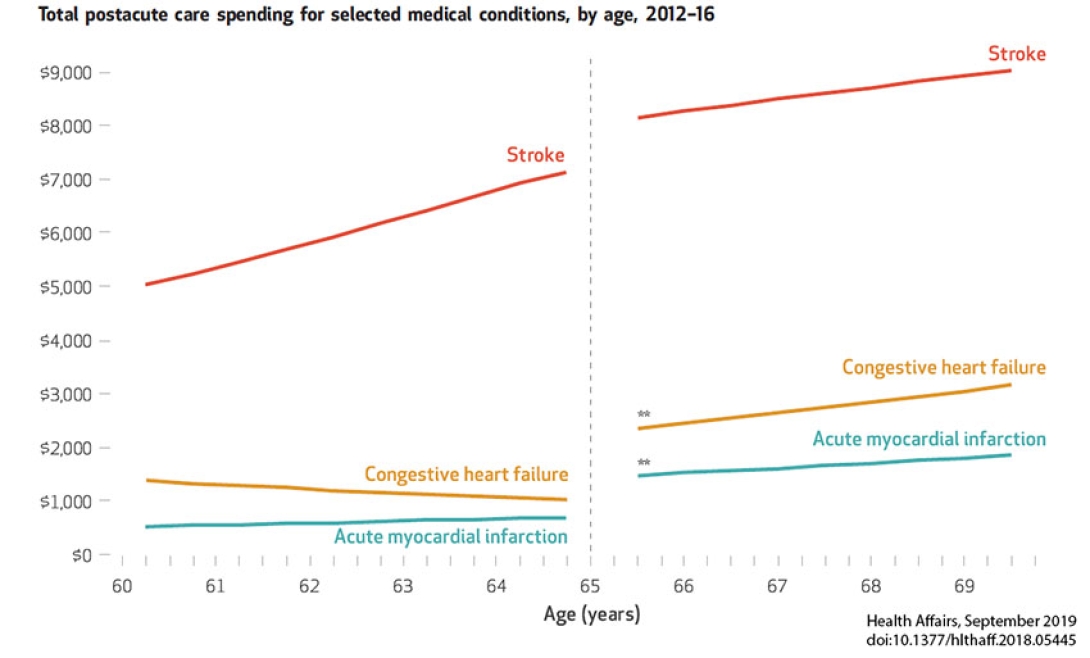
Yet, the differences in the percentage of patients who received any post-hospital care were relatively small. Instead, the largest differences were in the amount of spending among those who were prescribed care after hospitalization.
And despite this excess spending, the two groups had similar rates of readmission to the hospital within 90 days of leaving – a measure of how well a patient's recovery has gone.
"This shows that providers are making similar clinical decisions about what to do regarding post-hospital care for both types of patients, but that Medicare is far more permissive regarding the volume of services delivered and therefore the costs," says Scott Regenbogen, M.D., M.P.H., lead author of the paper, co-director of MVC and chief of colorectal surgery at Michigan Medicine, U-M's academic medical center.
"The only exception was stroke, where overall spending was similar between the two groups -- most likely because the clinical indications for stroke rehabilitation are so much more clear than in the other five conditions."
Change already starting
Regenbogen and his colleagues, including senior author Edward C. Norton, Ph.D., a U-M health economist, point out that Medicare covers post-hospital care provided within time-defined windows, while private insurance often sets coverage by day of overnight stay or outpatient or home visit. Private plans, working with the employers that pay for them, can set limits on exactly what they'll cover, or set co-pays to try to keep patients from using less-needed services.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
They also note that the Centers for Medicare and Medicaid Services, which oversees the Medicare system, has started to work to incentivize more judicious use of post-acute care in Medicare through the introduction of alternative payment models.
For instance, it has established 'bundled payment' programs that pay hospitals a set amount for the entire range of care that a hip or knee replacement patient needs, including post-hospital care. And Accountable Care Organizations are financially rewarded – and sometimes penalized – based on the total cost of care in and out of the hospital for the traditional Medicare patients who see the ACO's participating physicians.
More about the methods used
The new study grew out of the MVC team's general observations about the costs of post-acute care for patients with different forms of insurance whose hospitals take part in the consortium.
But in order to make a true comparison, the team had to peel away the layers of differences between the groups of patients so that they were clinically similar and prices of services were standardized. Those included weren't on Medicare for reasons such as kidney failure or disability that would have kept them off of private insurance before the age of 65.
The same approach could help researchers study differences between pre- and post-Medicare groups for other purposes.
Regenbogen and Norton are both members of the U-M Institute for Healthcare Policy and Innovation, as was the late Lena Chen, M.D., M.S., who is a co-author on the new paper and led a previous analysis of post-hospital care cost variation in Medicare participants. Other co-authors on the new paper are statistician Anne H. Cain-Nielsen from the U-M Department of Surgery, and John D. Syrjamaki from MVC.
Paper Cited: Scott Regenbogen, et al. "Spending On Postacute Care After Hospitalization In Commercial Insurance And Medicare Around Age Sixty-Five' Health Affairs. DOI: 10.1377/hlthaff.2018.05445
Funding: National Institutes of Health (AG019783; AG047860, AG047252, HS024698) and American Society of Colon and Rectal Surgeons.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





