Work requirements proposed in some states would probably apply to only a small group of Medicaid enrollees and may disrupt care for the chronically ill.
11:00 AM
Author |

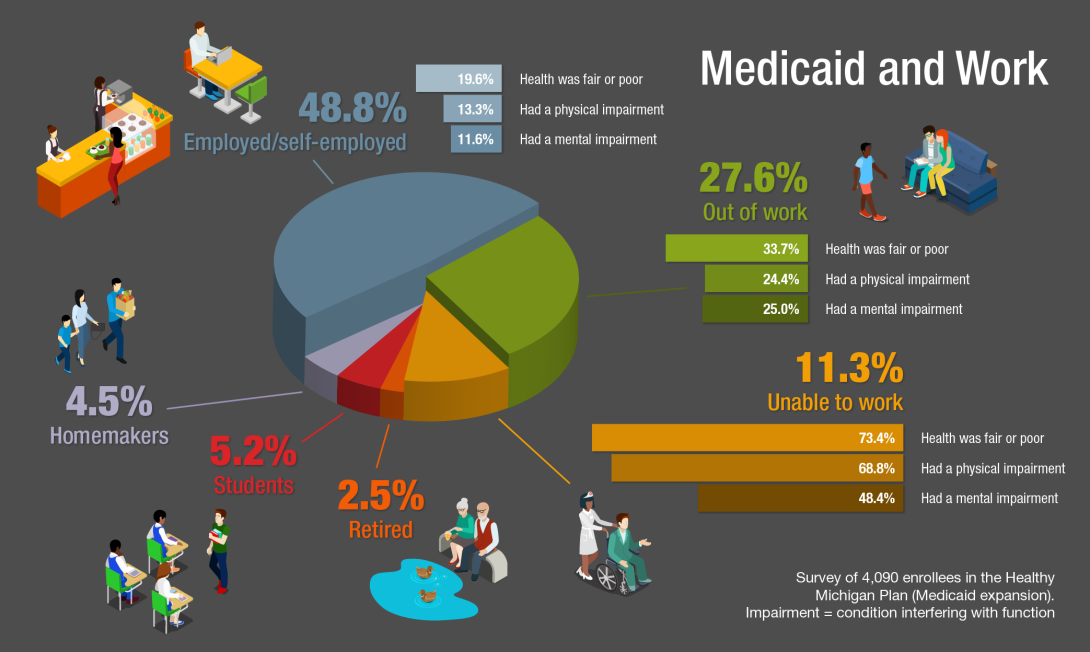
Nearly half of the people who enrolled in Medicaid after it expanded in Michigan have jobs, a new study finds. An additional 11 percent can't work, likely because of serious physical or mental health conditions.
MORE FROM THE LAB: Subscribe to our weekly newsletter
About 1 in 4 enrollees more are out of work but also are much more likely to be in poor health, according to findings published in JAMA Internal Medicine by a team from the University of Michigan Institute for Healthcare Policy and Innovation.
The findings, from a detailed 2016 survey of more than 4,000 people enrolled in Michigan's program for more than a year, might inform discussions of potential work requirements for the poor and near-poor Americans who qualify for expanded Medicaid in the 31 states and the District of Columbia that offer it, and other states that are considering expansion.
Several of those states have submitted proposals to require Medicaid expansion enrollees to work at least part time, actively seek work or volunteer, or risk losing Medicaid coverage.
Several others are considering doing so while the current federal administration has signaled a willingness to approve the waivers states need to enact such requirements. Some states have started voluntary work-referral programs for enrollees.
"The question raised by these data for states is: Is it worth the cost to screen and track enrollees when only a small minority isn't working who are potentially able to work?" says Renuka Tipirneni, M.D., M.Sc., lead author of the study and a clinical lecturer in general internal medicine at U-M.
"Even if they don't meet federal disability criteria, our survey shows many of these individuals face significant health challenges," she adds. "It's also important to consider that dropping them from coverage for failure to fulfill a work requirement could seriously impact their ability to receive care for chronic physical and mental health conditions that can worsen without treatment."
Health status and work
The study is the first published report about work-related information obtained directly from enrollees in Medicaid expansion states, rather than from administrative data or survey estimates.
SEE ALSO: Medicaid Expansion Helped Enrollees Do Better at Work or in Job Searches
It's also the first peer-reviewed study from IHPI's formal evaluation of Michigan's expansion, called the Healthy Michigan Plan. The evaluation, funded by IHPI's contract with the Michigan Department of Health and Human Services, is required under a federal waiver that allowed the state to customize its Medicaid expansion when it launched in April 2014.
Tipirneni and her colleagues, including senior author and IHPI Director John Z. Ayanian, M.D., M.P.P., and Susan D. Goold, M.D., M.H.S.A., compiled the report based on telephone surveys carried out in 2016 in a representative sample of Healthy Michigan Plan participants.
In all:
-
48.8 percent of respondents said they were employed or self-employed full or part time — though their incomes were all below 133 percent of the federal poverty level, about $15,800 for an individual and $32,300 for a family of four.
-
27.6 percent were out of work, in a state that in 2016 was around the national average for unemployment after a decade and a half of above-average unemployment.
-
One-third of those out-of-work respondents reported fair or poor health, compared with 19 percent among those who said they were employed.
-
Two-thirds of those out of work said they had a chronic physical illness, and 35 percent said they had been diagnosed with a mental illness.
-
One-quarter of those out of work said they had a physical or mental impairment that interfered with their ability to function at least half the days in the past month.
-
-
11.3 percent of respondents said they were unable to work. Of these, 73.4 percent reported being in fair or poor health.
-
2.5 percent said they were retired.
-
5.2 percent said they were students.
-
4.5 percent said they were homemakers.
Although the U-M team did not ask about respondents' roles as caregivers for other household members and how that may limit their ability to work, the researchers included these questions in the 2017 survey they just completed.
Respondents who had a mental health condition that limited their ability to function were twice as likely to be out of work. Other factors associated with individuals reporting not working included being in their 50s or early 60s, being male and being in fair or poor health overall.
Tipirneni notes that survey respondents who said they were employed or self-employed may have enrolled in the Healthy Michigan Plan because many low-wage jobs do not offer health insurance. Under the Affordable Care Act, employers are not required to offer health insurance if they have fewer than 50 workers or if their employees work fewer than 30 hours a week.
Those with incomes under the federal poverty level also cannot get financial help to purchase coverage through a health insurance exchange such as HealthCare.gov, whether their state expanded Medicaid or not.
"Medicaid expansion was designed to cover those who have a gap in their coverage or jobs that don't offer insurance but don't pay enough to allow someone to afford individual coverage," Tipirneni says. "States considering work requirements should evaluate their potential impact on individuals and the potential return on expenditures required for enforcement."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!