States must guide doctors in their new role certifying which patients are too sick to work or require caregivers, and take into account factors that could impact employability.
1:00 PM
Author |

New Medicaid rules in several states mean low-income people will have to work, or prove they're too unhealthy to work, to receive health coverage. Other states want permission to require the same, a move that could affect millions of Americans living in or near poverty.
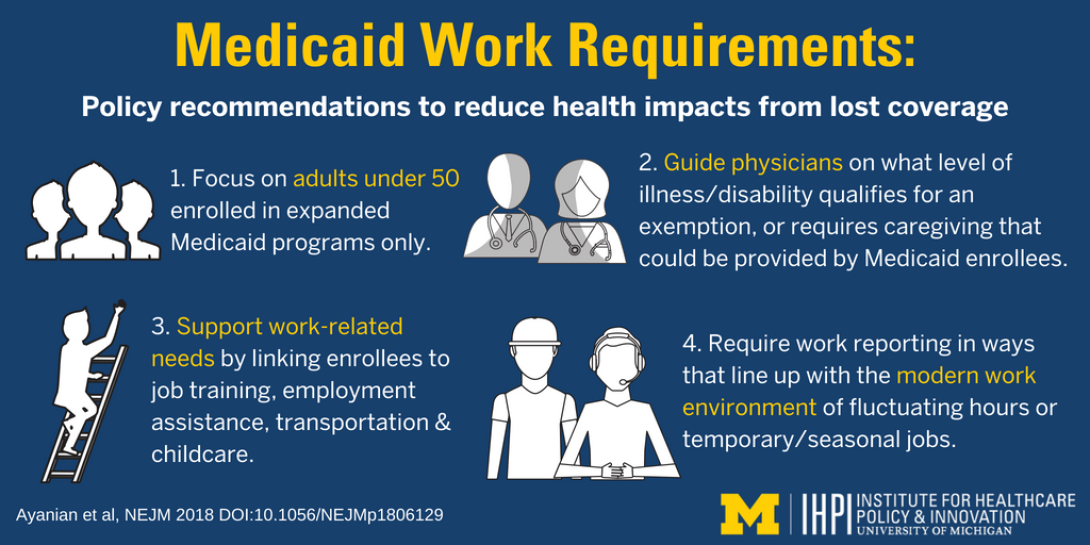
Before these requirements take effect, a team of University of Michigan researchers is offering specific recommendations to help states ensure that these work requirements don't harm the health of Medicaid enrollees.
The potential of harm as a result of losing Medicaid coverage forms the basis of a court case that has put Kentucky's Medicaid work requirement on hold and led to a public comment period that closes Aug. 18.
The U-M team, which has studied Medicaid for years, published its recommendations in the New England Journal of Medicine. The team's prior work on Michigan's Medicaid expansion showed that half of enrollees already work, and many others have health problems that limit their ability to work.
"We wanted to address the essential question: If we're going to have work requirements, then how can states implement them in the most humane way, so that the requirements focus on those who are more able to work and are less likely to experience worsening health if they lose coverage?" says John Z. Ayanian, M.D., M.P.P., lead author of the article and director of the U-M Institute for Healthcare Policy and Innovation.
"We based our recommendations on the evidence we have about the current Medicaid expansion population. We hope state policymakers will take our recommendations into account as they seek to create reasonable, sustainable programs."
Ayanian and his co-authors are all general internal medicine physicians who provide primary care to patients at Michigan Medicine, U-M's academic medical center.
If the goal is to help people improve their economic standing in life and become self-sufficient, they'll need support to do so.John Z. Ayanian, M.D., M.P.P.
Guidelines for successful implementation
The team's recommendations focus in part on the new role that physicians would play in states that implement Medicaid work requirements.
Among their suggestions:
Focus on adults under age 50 who enrolled in Medicaid expansions. Compared to people over 50 (and those under 50 whose health problems are serious enough to qualify them for traditional Medicaid), this population is less likely to suffer harm if the state bases their health insurance on their ability to work — or do another activity such as volunteering, attending school, undergoing addiction treatment or caring for a relative with a seriously illness or disability.
That's because research has shown they are less likely to have chronic health conditions or limits on their everyday function that could get worse if they lose their health insurance because they don't meet a work requirement. The team notes that Arkansas, which implemented a Medicaid work requirement June 1, already follows this recommendation.
Give doctors clear guidance. While doctors already play a key role in some certifications related to their patients' disability status or ability to do certain jobs, Medicaid work requirements would ramp up that role to include many more patients.
States, then, should make it clear to physicians exactly what health conditions and functional limits will make someone exempt from a work requirement — or what limitations a person must have to require the level of caregiving that a family member could provide in order to meet their work requirement. In the latter case, the physician certifying a patient's level of disability or need for caregiving could affect the health insurance coverage for the patient's caregiver — potentially someone not in that doctor's direct care.
The new requirements may increase the workload for physicians and their staffs appreciably, the U-M authors note.
Support work-related needs. Although the Medicaid system itself cannot pay using federal funds for services such as job training, help finding a job, or help getting to and from work or caring for children while a parent works, states adopting the new work requirement should connect Medicaid enrollees to such services, the team says.
Such services would improve the odds that people covered by Medicaid will be able to find and keep jobs that will allow them to meet their state requirement, or even find a job that pays enough or provides health insurance benefits so that they no longer need Medicaid.
Make work reporting line up with today's work environment. As more workers have work patterns with hours that fluctuate week to week, have occasional gaps due to temporary jobs, or obtain seasonal employment, states should take this into account in their Medicaid reporting requirements, the team says.
Requiring that participants report their work histories less frequently, covering a longer period of time, could smooth out these fluctuations and reduce the chance that a person who is making an effort to work will have to leave the Medicaid program.
Support systems remain crucial
Ayanian and co-authors Renuka Tipirneni, M.D., M.S., and Susan Goold, M.D., M.A., MHSA, note that as work requirements become more widespread as part of ongoing or new Medicaid expansion programs, the details of implementation will become more important. All are faculty members in the Division of General Internal Medicine at the U-M Medical School and are members of IHPI.
"If the goal is to help people improve their economic standing in life and become self-sufficient, they'll need support to do so," says Ayanian, who also holds faculty appointments in the U-M Ford School of Public Policy and School of Public Health.
"States should prevent potential harm that will arise if people with chronic conditions lose their Medicaid coverage and therefore their access to health care providers and medications, especially if the economy changes."
Adds Goold: "If the goal is to provide a 'leg up' to economic self-sufficiency rather than a 'hand out,' providing health insurance through Medicaid is just one piece of providing such support. Child care, transportation, education and training, as well as health issues, present obstacles to self-sufficiency."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!