U-M findings from an official Healthy Michigan Plan evaluation show a slice of the ACA’s financial impact on hospitals in the state.
7:00 AM
Author |
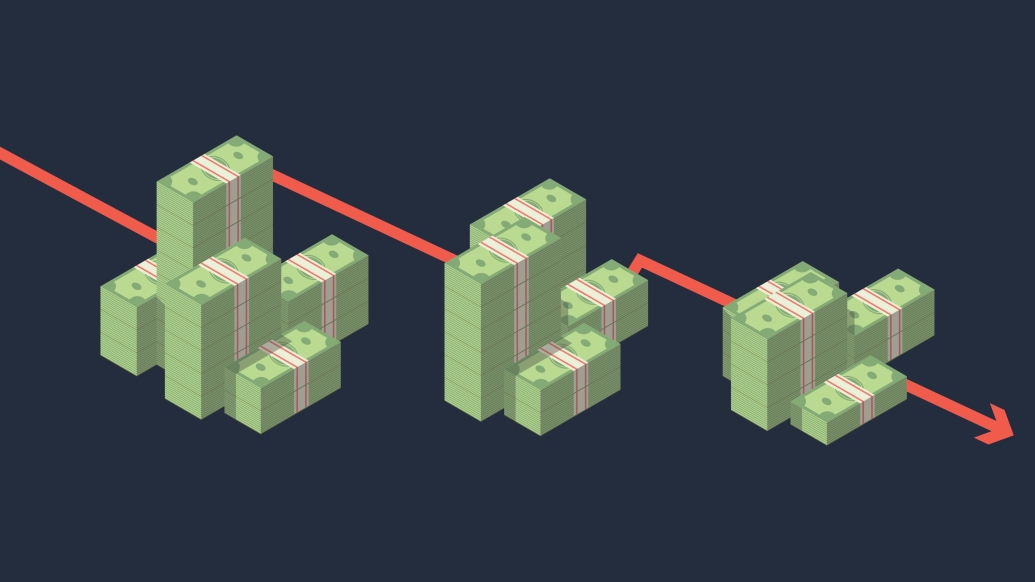
For decades, hospitals have written off the cost of hundreds of millions of dollars' worth of health care every year after caring for people who didn't have health insurance. The cost, from unpaid bills and charity care, weighs on the finances of these institutions.
MORE FROM THE LAB: Subscribe to our weekly newsletter
But a new University of Michigan study shows that soon after the state government expanded Medicaid under the Affordable Care Act in spring 2014, many hospitals in Michigan saw a major drop in this care.
For the 88 hospitals reporting a full year's worth of data from the post-expansion era — 62 percent of all hospitals in the state — the amount dropped by about half overall. Although not all of the hospitals saw such a large decrease, more than 90 percent saw a decline in the percentage of their expenses that came from uncompensated care.
In 2013, hospitals spent about 5.2 percent of their budgets on writing off the cost of unpaid care, absorbing $627 million. In 2015, it was down to 2.9 percent and $327.1 million.
Researchers from the U-M Institute for Healthcare Policy and Innovation conducted the analysis and published it in an official report to the state and federal governments.
"What we see in the group of hospitals for which we have full data is a dramatic decrease in uncompensated care after Medicaid was expanded," says Thomas Buchmueller, Ph.D., one of the leaders of the new analysis and a professor at the U-M Ross School of Business.
Adds co-author Helen Levy, Ph.D., a research professor at the U-M Institute for Social Research, "The decline occurred across the board. Nearly every hospital in our sample saw a drop in uncompensated care between 2013 and 2015. We will continue to monitor this trend as more data become available."
Two kinds of unpaid care
Uncompensated care includes both charity care and bad debt. Hospitals provide charity care for patients who meet their criteria, without expecting to be paid, and account for what the care cost them. The Affordable Care Act includes requirements for hospitals regarding charity care, though a 2015 IHPI study found that many had not yet fully complied in the first year of the requirement.
Also included in uncompensated care is bad debt, or the total amount of uncollected bills that the hospital issues to patients.
Bad debt can come from patients who have no insurance but who have incomes that the hospital deems high enough to make payment feasible. It can also come from patients who have insurance that does not cover the entire cost of their care, such as those with high-deductible plans (often called underinsurance, when an insured patient owes more money than he or she can pay).
Reporting results
The IHPI holds the state contract to conduct a federally mandated evaluation of Healthy Michigan Plan's impact on the state's population, health care system and government. That plan began in April 2014 and covers about 638,000 low-income Michiganders.
SEE ALSO: Medicaid Expansion More Than Pays for Itself, Study Finds
Most participants in the plan were uninsured before enrolling. The maximum income a single adult can make and still enroll in the plan is about $16,400 per year. Federal funds under the Affordable Care Act mainly support the plan, though the state started paying 5 percent of costs in the fiscal year that began in October.
Levy, IHPI Director John Ayanian, M.D., M.P.P., and colleagues recently published a study of the plan's economic impact in the New England Journal of Medicine, conducted separately from the state-contracted evaluation. It showed that the Healthy Michigan Plan has generated an economic impact that supports more than 30,000 new jobs every year and creates about $2.3 billion more in personal spending power each year for Michigan residents.
The new data come from analyzing official reports that hospitals submit to Michigan's Medicaid program. Because hospitals observe different fiscal years, data from all hospitals' fiscal year 2015 reports were not available in time for the U-M team to include in the analysis.
The researchers also compared data from all 142 Michigan hospitals for fiscal year 2013 and fiscal year 2014, which includes the start of Medicaid expansion. This analysis shows a drop in uncompensated care from $1.1 billion to $913.5 million, and a drop in the percentage of hospital expenses attributed to uncompensated care.
To see data from each of the 142 hospitals that report uncompensated care costs to the state, view this PDF file on the IHPI website. The full IHPI-written report on uncompensated care and other aspects of the Healthy Michigan Plan's impact is available on the state website.
In addition to Buchmueller and Levy, the authors of the report include Jordan Rhodes, Ph.D., of U-M's Ross School of Business, and Sayeh Nikpay, Ph.D., M.P.H., a former IHPI research fellow now at Vanderbilt University. Kyle Grazier, Dr.P.H., M.P.H., M.S., and Charley Willison, of the U-M School of Public Health, also conducted an analysis of insurance premium rates since implementation of the Healthy Michigan Plan.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!