A new digital tool offers an evidence-based guide to vascular access devices that could change bedside decisions — and boost patient safety.
7:00 AM
Author |
More than a million times a year, doctors and nurses insert tiny tubes into the veins of American hospital patients to deliver lifesaving medicines, give fluids and nutrition, and monitor key vital signs.
MORE FROM THE LAB: Subscribe to our weekly newsletter
The devices, used for ongoing vascular access, help patients with conditions ranging from cancer and pain to serious infections.
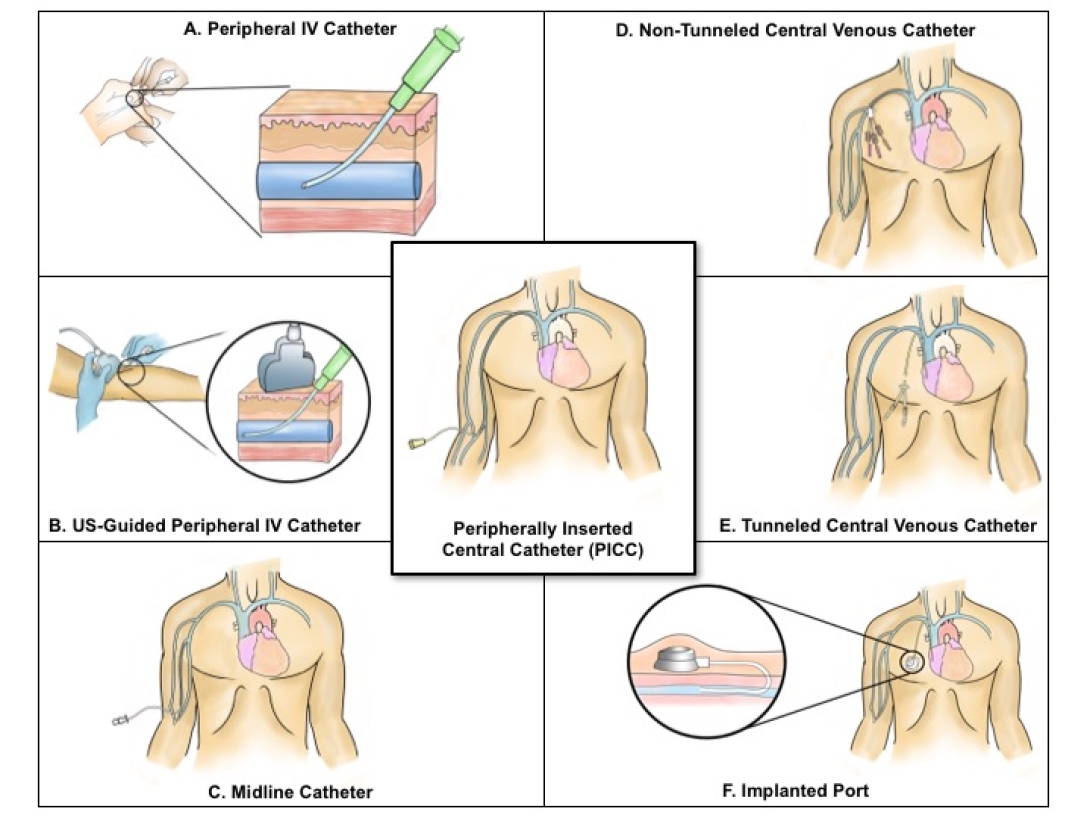
But these devices carry risks as well as benefits — especially peripherally inserted central catheters (PICCs), which are designed to stay in the body for days or weeks. PICCs tunnel deep into the bloodstream, providing a gateway for microbes and a place for dangerous clots to form.
Yet despite the widespread and rapidly growing use of such devices, doctors and nurses have only recently had an evidence-based guide for choosing which device to use, in which patient, for the best and safest result — and which to avoid at all costs.
A team at the University of Michigan and VA Ann Arbor Healthcare System created the guide, called the Michigan Appropriateness Guide for Intravenous Catheters (MAGIC). Two years ago, the team published it for all to use and created ImprovePICC.com as a one-stop resource on the latest recommendations for clinicians.
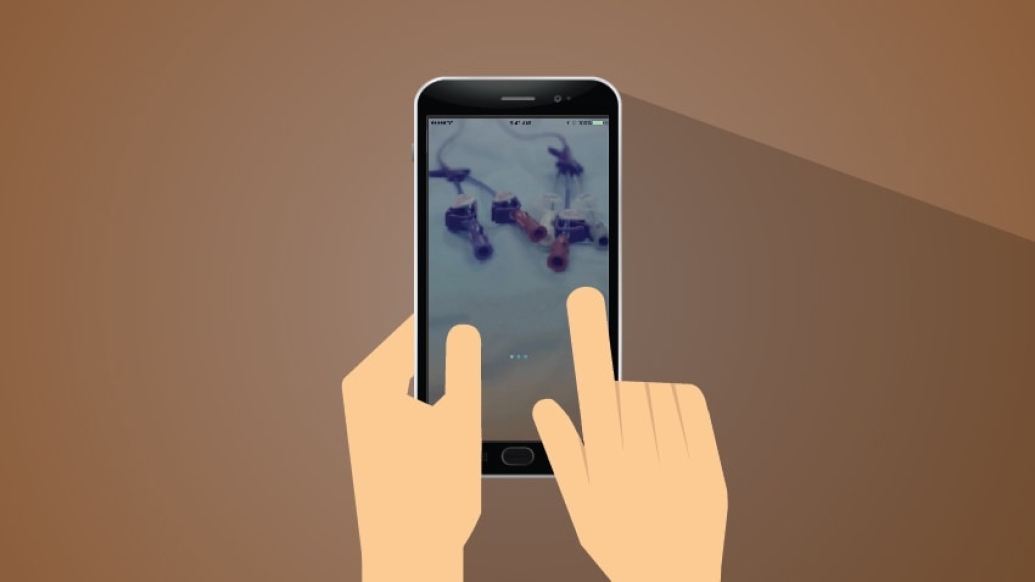
Now, the guide is available as a free smartphone app for both Apple iOS and Android devices, helping clinicians at the point of care choose among intravenous or vascular access devices of all kinds.
These devices have become especially convenient to place, and their use has gone up dramatically — as have rates of complications.Vineet Chopra, M.D., M.Sc.
Creating MAGIC
"These devices have become especially convenient to place, and their use has gone up dramatically — as have rates of complications," says Vineet Chopra, M.D., M.Sc., who spearheaded the MAGIC effort. "This app will make it even easier for clinicians to know when the use of a PICC is appropriate and when other choices are the best."
PICCs and other such devices are commonly used by clinicians in many fields, including vascular nursing, anesthesiology, radiology, critical care, hospital medicine, infectious disease and oncology.
The MAGIC guide grew out of top international experts across these fields, an evidence review and research at the U-M/VA Patient Safety Enhancement Program that revealed the hazards of some PICC use.
Criteria are based on experts' review of more than 600 scenarios of patients and treatments. The 47 Michigan hospitals taking part in the Michigan Hospital Medicine Safety Consortium, a patient safety project, are testing the system.
Previously, data from the consortium revealed huge variation between hospitals' use of IV devices for the same conditions. Evidence from this collaborative effort also shows that patients with PICCs frequently face a risk of deep vein thrombosis.
SEE ALSO: Can Cancer Cause Blood Clots?
Going forward, the U-M/VA team will test ways to deploy MAGIC across the Veterans Affairs health system, working with the VA National Center for Patient Safety and the No Preventable Harms campaign. The Infusion Nursing Society also updated its standards to incorporate changes based on MAGIC's recommendations.
"IV devices of all kinds are being put into patients without much thought about risks, benefits or alternatives. At the end of the day, MAGIC gives providers the information they need to make a good decision for their patient — one that will render these devices appropriate and safe," says Chopra, a professor and chief of the new Division of Hospital Medicine in the Department of Internal Medicine at Michigan Medicine, the U-M academic medical center.
The work is supported by the Society of Hospital Medicine, the Agency for Healthcare Research and Quality, and Blue Cross Blue Shield of Michigan, which funds the Michigan Hospital Medicine Safety Consortium.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!