Research and Policy Media Relations Manager
Gavin draws on more than 25 years of experience in communicating about science, medicine and health policy. She focuses mainly on the health services research done by members of the U-M Institute for Healthcare Policy and Innovation, who work to understand and improve the safety, quality, equity and affordability of health care. As part of the Michigan Medicine communication team, she has lead responsibility for primary care and mental health topics. Contact: [email protected]; Twitter: @Karag


Health Lab
Advanced programs in healthcare equip doctors, nurses, and others with the skills and knowledge needed for successful careers in health. Explore how Michigan’s Clinician Scholars Program can empower healthcare innovators across different disciplines and enhance medical education.
News Release
Puts focus on population-based patient care from birth to end of life, developing core areas of research and training a new generation to lead primary care tomorrow
News Release
A neuroscientist who began his career at the University of Michigan and made important inroads in understanding the mysteries of sleep has returned to Ann Arbor to lead a fast-growing community of scientists studying the brain, nervous system and mind.
Health Lab
Screening primary care patients for gun ownership has been recommended especially for people with mental health issues. A Michigan Medicinestudy shows wariness by providers and patients.

Health Lab
Firearm purchases rose during the pandemic and a survey shows high rates of mental health issues and political extremism among those who bought guns during 2020 and 2021.
Health Lab
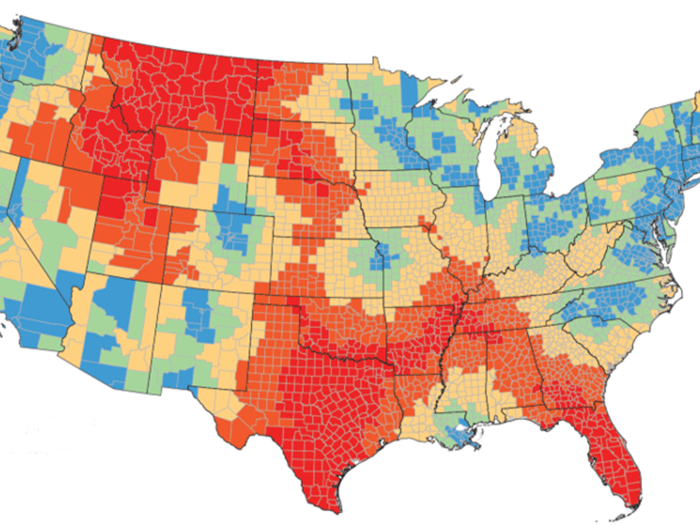
Medicaid expansion’s impact on low-income Michigan residents included reduced uninsurance, increased primary and preventive care, and better financial health.
Health Lab
Few children are getting eyes checked at their pediatrician or other regular doctor’s office, and rates vary greatly by insurance status.

Health Lab
RSV vaccines are now available to older adults for the first time; a poll gauges awareness and interest among those over 60.

Health Lab
Mammograms, Pap tests, colonoscopies and lung CT scans have the power to detect cancer early and save lives – a new study tallies up the savings in both years and dollars.
Health Lab
People with chronic pain who take opioids have trouble finding multimodal pain care; insurance and provider education changes are needed, experts say

Health Lab
Needs related to housing, transportation, food, social support and more can be identified through AI/ML techniques
Medicine at Michigan
A 1999 story in Medicine at Michigan was hopeful about the expansion of telemedicine — a promise that would not be realized until 2020.

Health Lab
A link between vision issues in older adults and an increased likelihood of dementia.
Health Lab
Access to mental health care has lagged even as diagnoses have risen; a proposed federal fix aims to increase insurance coverage of care.
Health Lab
Gender-affirming care for transgender teens is restricted or may be soon in 20 states; this has increased travel time to available clinics