A Michigan Medicine expert describes the science behind the most promising vaccines for the coronavirus pandemic.
5:00 AM
Author |

Editor's note: Information on the COVID-19 crisis is constantly changing. For the latest numbers and updates, keep checking the CDC's website. For the most up-to-date information from Michigan Medicine, visit the hospital's Coronavirus (COVID-19) webpage.
Interested in a COVID-19 clinical trial? Health research is critical to ending the COVID-19 pandemic. Our researchers are hard at work to find vaccines and other ways to potentially prevent and treat the disease and need your help. Sign up to be considered for a clinical trial at Michigan Medicine.
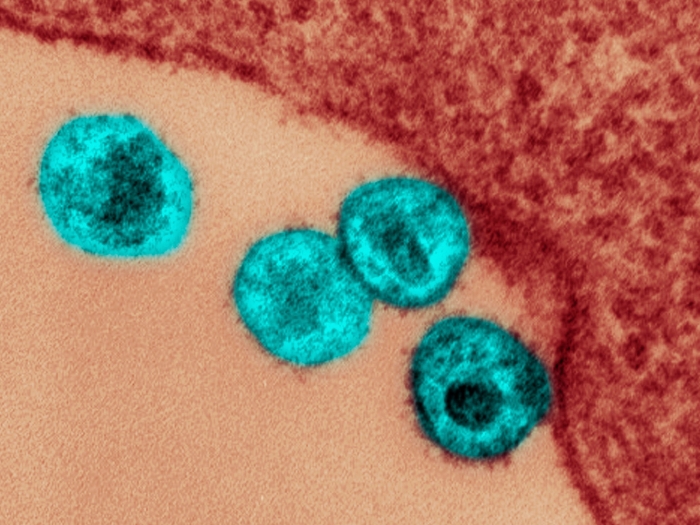
The U.S. government's Operation Warp Speed is a science fiction sounding name for a very real challenge: developing a vaccine in record time to end a pandemic. As a result of the combined efforts of thousands of scientists around the world, a list of over 100 potential vaccines has come down to a promising few that are soon entering large clinical trials. But what are these vaccines and how would they work?
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily updates on iTunes, Google Play and Stitcher.
Adam Lauring, M.D., Ph.D., associate professor of internal medicine and microbiology and immunology at the University of Michigan Medical School, weighs in on the leading five vaccine candidates for COVID-19, described in a recent issue of the Journal of the American Medical Association:
Two of the vaccine candidates (from Johnson & Johnson/Janssen Pharmaceuticals and AstraZeneca/University of Oxford) use something called an adenovirus. What is that and why is it used?
Adenoviruses are viruses that can cause the common cold. We as humans have them, monkeys have them, as do other animals. For years, people have been using these viruses to deliver DNA, which are instructions for proteins. For the COVID-19 vaccine, researchers swap in a gene from SARS-CoV-2. When the vaccine is given to someone, the modified cold virus makes the SARS-CoV2 protein, which stimulates the immune response.
Can you get sick from the SARS-CoV2 protein or the modified virus?
No, the protein can't make you sick. The virus does its job and then it goes away. There will always be a lot of attention to safety. Everything we know about how viruses grow and make proteins is controlled when you design a vaccine.
Is using a virus to deliver DNA to cells a new technique for making a vaccine?
Using viruses to vector, or deliver DNA, has been around for a couple of decades. For example, for the Ebola virus, they used a different virus to deliver a protein and that was shown to be effective.
One company is using a cold virus from a monkey to deliver DNA while another is using a human cold virus. Why?
Each company kind of develops its own system, but the rationale is the same: Find a virus that not a lot of people have been exposed to before. By using a monkey adenovirus, a human won't have been exposed to it. In humans, there are a lot of different types of adenoviruses, some a lot more common than others. The vaccine is likely made from a rare one. If you use a common virus, there's always a chance someone will have been infected naturally and their immune system will attack the vaccine before it can work.
One of the vaccine candidates (from Merck, Sharpe & Dohme/International AIDS Vaccine Initiative) uses recombinant vesicular stomatitis virus. What is that?
Vesicular stomatitis virus is a virus that primarily infects livestock (cows, horse, pigs). Here, it is being used as a vector delivery system, much like the human or chimpanzee adenoviruses. The modified vesicular stomatitis virus delivers the instructions for the SARS-CoV-2 protein into cells. This recombinant candidate works really well against Ebola and has been proven in the field; people developed immunity to Ebola pretty quickly after getting vaccine.
The final two vaccine candidates (from Moderna and BioNTech/Fosun Pharma/Pfizer) are mRNA vaccines. What are those?
First it helps to remember that DNA is the gene and RNA gives instructions for certain proteins. So an mRNA vaccine is the instructions for the SARS-CoV2 protein. Once inside the cell, the protein is made and that triggers the immune response. Just like the vector vaccines which use viruses to deliver the protein instructions, here you are delivering the instructions alone. It's another way of getting the protein made inside of you.
How will we know if the vaccines work?
With most vaccines, people talk about correlates of protection – what you observe and the immune response are correlates or predict whether you will be immune or not. With most vaccines in the past, such as the vaccines for measles, hepatitis B and seasonal flu, a good antibody response is correlated with being protected. Specifically, something called a neutralizing antibody response prevents the virus from infecting the cell.
Are antibodies the only form of immune protection?
No. We do know that other immune responses are important and helpful. One, to develop a good antibody response it helps to have a good T cell response. T cells in your immune system help stimulate B cells, which can make antibodies better. There's also parts of your immune system that you can train so that they recognize when a cell is infected with the virus so that your immune cells can kill them off. A lot of these vector vaccines are thought to be good at triggering multiple arms of the immune system.
Is there any risk of getting COVID-19 or COVID-19-like side effects from these vaccines?
When people talk about side effects of a vaccine, people often believe you're getting a weaker version of the virus and a minor version of the disease. That is not what these things do. Most vaccine side effects — which include anything from a sore arm, to feeling warm to muscle aches — are a sign of the immune response. It's not that you get a mild form of the disease. That's important to be clear about. People keep a very close eye because you want to make sure these vaccines are safe.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
Paper cited: "Developing a SARS-CoV-2 Vaccine at Warp Speed," JAMA. DOI: 10.1001/jama.2020.12190

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!