A study including more than 4,000 people with either type 1 or type 2 diabetes — all under age 21 — revealed a troubling eye health trend.
11:00 AM
Author |
Blindness and eye problems may seem far in the future for children and teenagers with diabetes. But a new study shows these concerns shouldn't be overlooked in those with the condition — of any age.
MORE FROM THE LAB: Subscribe to our weekly newsletter
The large, national study, led by University of Michigan Kellogg Eye Center, shows more than 1 in 5 youth with type 1 diabetes, and 7 percent with type 2 diabetes, have diagnoses of diabetic retinopathy, a weakening of the walls of the eye's blood vessels after prolonged exposure to high blood sugar. In the review of 4,008 cases, children as young as 6 had been diagnosed with proliferative diabetic retinopathy, the more advanced form of the disease.
Those in the study, which was published in Ophthalmology, were all enrolled at 21 or younger.
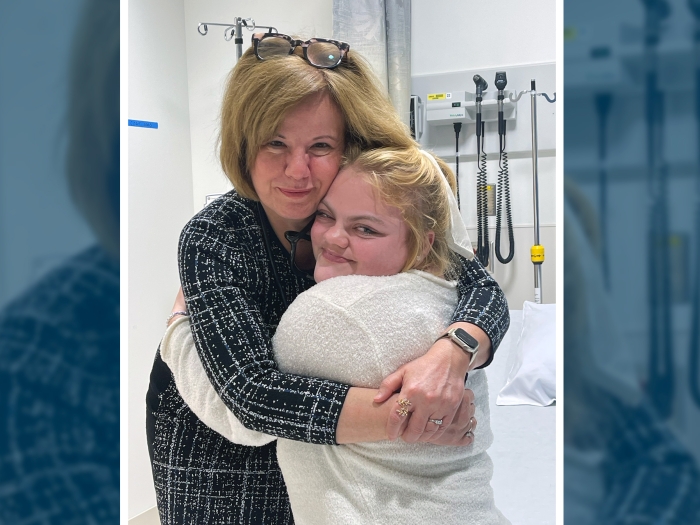
"There is a perception that diabetic retinopathy is very uncommon in youth, but there's reason to believe they are at considerable risk," says Sophia Y. Wang, M.D., the study's lead author and a resident physician at Kellogg Eye Center.
In the past, most kids keeping track of their blood sugar had the type 1 form. But today, type 2 diabetes accounts for nearly half of all new diabetes cases among adolescents, a climb concurrent with the rise of obesity and inactivity among kids.
The researchers wanted to know more about risk factors for developing diabetic retinopathy in this age group, and whether screening guidelines would adequately catch signs of diabetic retinopathy in time to preserve a child's sight.
They learned those with uncontrolled blood sugar — measured by HbA1c levels — jeopardized their vision. For every 1-point increase in HbA1c, risk for diabetic retinopathy increased 20 percent for those with type 1 diabetes, and 30 percent among those with type 2 diabetes.
The main reason people with diabetes are encouraged to have regular eye exams is to look for changes in the blood vessels of the retina. The early stages of diabetic retinopathy don't cause changes in vision, but a dilated eye exam can reveal changes in the back of the eye.
Current guidelines suggest that ophthalmic screening begin three to five years after an initial diabetes diagnosis. By that time point in the study group, however, more than 18 percent of those with type 1 diabetes had already received a diabetic retinopathy diagnosis.
This suggests a troubling result, and a missed opportunity to detect diabetic retinopathy in its early stages to prevent irreversible retinal damage and preserve sight.
There is a perception that diabetic retinopathy is very uncommon in youth, but there's reason to believe they are at considerable risk.Sophia Y. Wang, M.D.
A call for more research
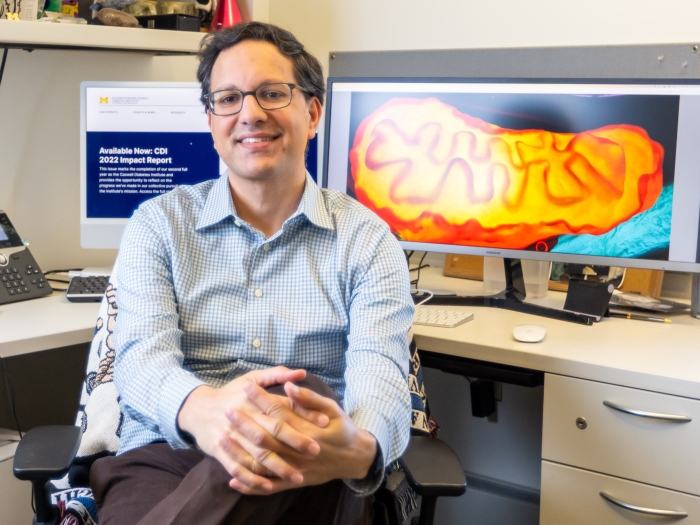
Wang and her co-authors, including University of Michigan Medical School associate professor of ophthalmology Joshua Stein, M.D., M.S., suggest more research is needed to better understand the ideal timing of screening.
SEE ALSO: Telemedicine Could Improve Eye Exam Access for People with Diabetes
"We hope our study will help inform pediatricians and other health care providers who care for youth with diabetes about the importance of referrals to an ophthalmologist or optometrist to check for retinopathy," says Stein, a member of the U-M Institute for Healthcare Policy and Innovation and director of the Center for Eye Policy and Innovation.
The checks should happen at least as often as the current guidelines, but there may be high-risk groups, such as those with worse glycemic control, who would benefit from earlier screening, he says.
As more adolescents are diagnosed with diabetes, it's worth developing new ways to monitor them for diabetic eye problems that are convenient for patients and their parents, he adds.
This might include telemedicine appointments where eye specialists can examine patients remotely or get images, taken during a primary care appointment, sent to them digitally.
In addition to Wang and Stein, the Michigan Medicine research team included statistician Chris A. Andrews, Ph.D., William H. Herman, M.D., M.P.H., professor of endocrinology, and Thomas W. Gardner, M.D., M.S., professor of ophthalmology. Stein and Herman also hold joint appointments in the U-M School of Public Health.
Research to Prevent Blindness, W.K. Kellogg Foundation, Juvenile Diabetes Research Foundation, the Taubman Institute, Michigan Diabetes Research Center and the Janssen Research Foundation funded the research. The data from the study was from the Clinformatics Data Mart created for Optum Inc. and includes information from people enrolled in a nationwide managed care organization from 2001 to 2014.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!