With more veterans than ever getting health care outside the VA system, there are new efforts to train medical students, residents and medical school faculty about vets’ special needs.
7:00 AM
Author |

Veterans Day is an important chance to remember that 70 percent of our veterans — including many of the 2.5 million who served in Iraq and Afghanistan — get their health care outside the Veterans Affairs (VA) health-care system.
MORE FROM THE LAB: Subscribe to our newsletter
The VA has expanded its program to cover non-VA care as part of efforts to boost access to care. So, perhaps without even knowing it, civilian doctors, nurses and other health professionals are treating many of those who served in the military.
Other factors have changed the care veterans need, too. For one, more veterans are women than in previous generations — 2.2 million in all.
At the University of Michigan Medical School, students studying for careers in medicine and other health professions can get new training to help them understand how a veteran's experience in the military can influence his or her health. Medical school faculty are also getting lessons in veteran-centered care, lessons that are now available to everyone through a free U-M online course.
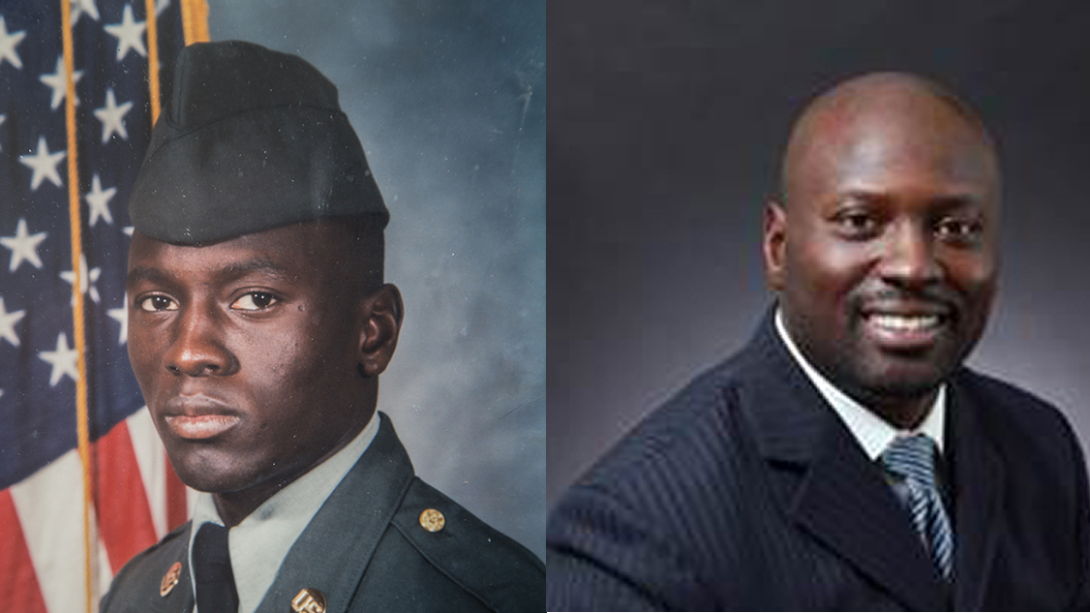
Last year, the team behind this effort published a photo piece in the Journal of Women's Health showing veterans "then and now" — during their service and today. Some of the works are featured in this article.

U-M Medical School professor and VA Ann Arbor Healthcare System leader Monica Lypson, M.D., MHPE, and medical education project manager Paula Ross, Ph.D., led that effort.
They hope to call attention to the commitment medical schools must make to improve veteran care training for the students who are tomorrow's health care providers.
Treating veterans outside the VA
The team notes that health care providers need to ask all patients four military-specific history questions:
-
Did you, or someone close to you, serve in the military?
-
When did you serve?
-
Where did you serve?
-
What did you do in the military?
Asking all patients about previous military service can help ensure that patients get the care they deserve from a team that understands them better.
If a health care provider doesn't ask, a veteran shouldn't hesitate to volunteer the information, the team adds.
With nearly 15 years as a staff physician at the Ann Arbor VA and expertise as a medical educator, Lypson has seen firsthand the important gaps in training necessary to improve care to veterans.
"Each year, tens of thousands of health professional trainees enter the VA health care system with limited knowledge or training about the military or veterans," she says. "As educators, we have to do better at preparing our learners for this increasing population both inside and outside the VA health care system."
As educators, we have to do better at preparing our learners for this increasing population, both inside and outside the VA health care system.Monica Lypson, M.D., MHPE
As a combat veteran of Operation Desert Storm, Ross says, "I've always seen civilian physicians, and in over 20 years as a veteran, not one has ever asked me about my military service."
SEE ALSO: A New Theory on What's Really Happening in PTSD Brains
In reaction to some of these photos, U-M medical student Kathryn Goldrath wrote in the Journal of Women's Health article, "As a medical student preparing for clinical rotations at the VA, I often wondered how I could empathize with my veteran patients, understanding minimally about the VA systems, military service and unique health needs of this population.

"Reflecting on these images with educators and classmates in a small-group setting helped me articulate and reconcile my own unvoiced biases that I may bring into a medical encounter, opening a space for more thoughtful discussion about the medical, psychological and social trajectory of a veteran's life.
"Prior to my exercise, if I had encountered some of the individuals in these photographs outside of the VA, I may not have thought to ask about a military history and may have potentially missed an important part of their patient history. The images reinforce the need for viewers to develop a patient-centered approach in any patient interaction, understanding that there is always a story beyond what we observe."
In this vein, writing in the Journal of Graduate Medical Education, Lypson, Ross and others reported findings from a survey of new medical residents about their understanding of veteran-related issues.
In all, two-thirds of those surveyed had had some experience at a VA hospital during medical school — but only one percent were veterans themselves. And the respondents' knowledge of two key issues for recent veterans — post-traumatic stress disorder and military sexual trauma — was lacking.
Together with these results, the team offers a model for training medical students and residents in veterans' health.
They write, "Educating trainees in military culture will hopefully improve their ability to recognize and diagnose symptoms, which is expected to reduce the problem of service members 'slipping through the cracks' and not receiving proper care. Through these efforts, we hope to address the larger mission, which is to train physicians to serve those who have served us."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!





