A new discovery about a common and potentially deadly bacterium could one day pave the way for new, needed antibiotics.
7:00 AM
Author |
When a patient battles invading bacteria — from pneumonia, say, or even an infected cut — the outcome may hinge on a microscopic arms race for an essential element: iron, which bacteria need to replicate and cause disease.
MORE FROM THE LAB: Subscribe to our weekly newsletter
Now, scientists from the University of Michigan Medical School say they have figured out how this process actually increases the risk from one of our most dangerous microscopic foes, Klebsiella pneumoniae. They made the discovery in mice with pneumonia.
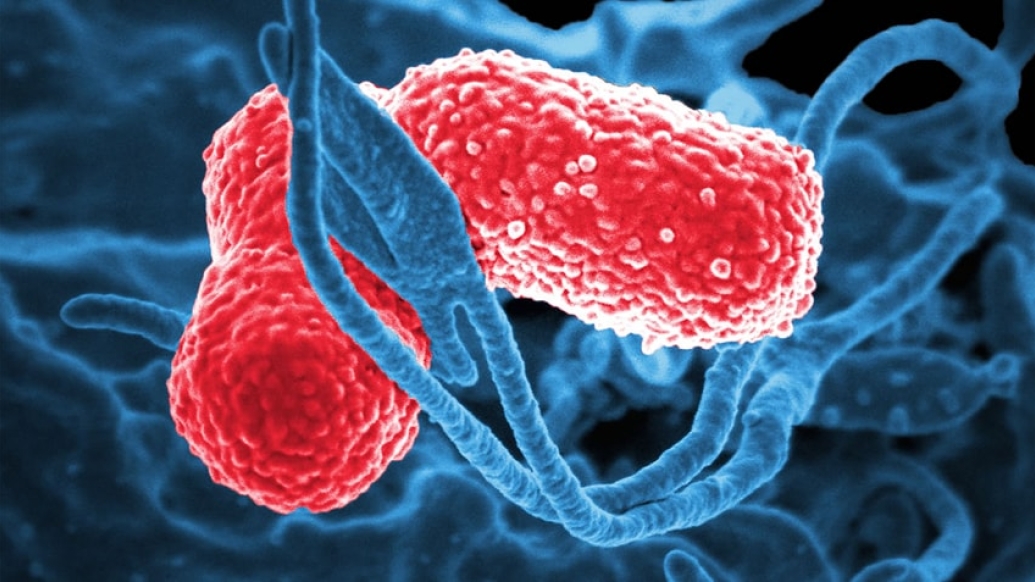
K. pneumoniae has already figured out how to overcome our best defenses — including, in some cases, all the most-powerful antibiotics.
It's the third-most-common cause of infections that arise in hospitalized patients, and it causes pneumonia, urinary tract infections, wound infections and bloodstream infections. In its most drug-resistant form, it's one of the carbapenem-resistant Enterobacteriaceae, or CRE — so-called "nightmare bacteria."
The new findings could aid the search for drugs to fight it and other superbugs.
This is a bacterium that has evolved new ways to get iron, and it turns out that the mechanism it uses also causes cellular stress during infections.Michael Bachman, M.D., Ph.D.
Iron scavenging — and more
In a new paper in the journal mBio, the team led by Michael Bachman, M.D., Ph.D., reports what happens after the bacteria send out tiny, iron-scavenging molecules.
SEE ALSO: To Improve Response During Outbreaks, Tap the Hive Mind
Called siderophores, those molecules have long been thought of as a way for bacteria to gather a precious element needed to grow and reproduce, by attaching to iron and stealing it from human bodies.
Siderophores from K. pneumoniae are hundreds of times more powerful at grabbing iron than the proteins our own bodies produce. What's more, the bacteria produce a kind of siderophore our immune systems can't neutralize.
But Bachman and his colleagues show that bacterial siderophores do much more than just grab iron. Their experiments show that K. pneumoniae actually uses the molecules to help invade the rest of the body beyond the initial point of entry and to bring on inflammation our own immune systems cause.
"This is a bacterium that has evolved new ways to get iron, and it turns out that the mechanism it uses also causes cellular stress during infections," says Bachman, an assistant professor of microbiology at U-M. "That response triggers an immune response that tells our bodies to fight the infection, but it also activates a mechanism that allows bacteria to escape and travel to the rest of the body."
That mechanism, a protein called Hif-1alpha, normally helps our bodies respond to low oxygen or iron. But when K. pneumoniae siderophores activate it, it worsens the infection. Exactly how is still a mystery.
SEE ALSO: Surgery Surprise: Small, Rural Hospitals May Be Safer for Common Operations
Bachman sees K. pneumoniae's effect on patients in his work as a clinical pathologist at the U-M Health System, where he's associate director of clinical microbiology. That motivates him to study it in the lab, though he notes it's too early to say exactly how the discovery could be used to help patients.
One promising route could be developing strategies to prevent the bacteria from sending out siderophores in the first place — or to use the siderophores to bring antibiotics back into bacterial cells. It may even be possible to create a vaccine based on siderophores to teach the immune system to attack them as invaders.
Meanwhile, he and others at U-M including microbiology and immunology chair Harry Mobley, Ph.D., are pursuing a broader goal through U-M's Host Microbiome Initiative. Using an advanced genetic technique called transposon sequencing, they're studying which genes K. pneumoniae and other superbugs absolutely need to cause infections.
The methodology
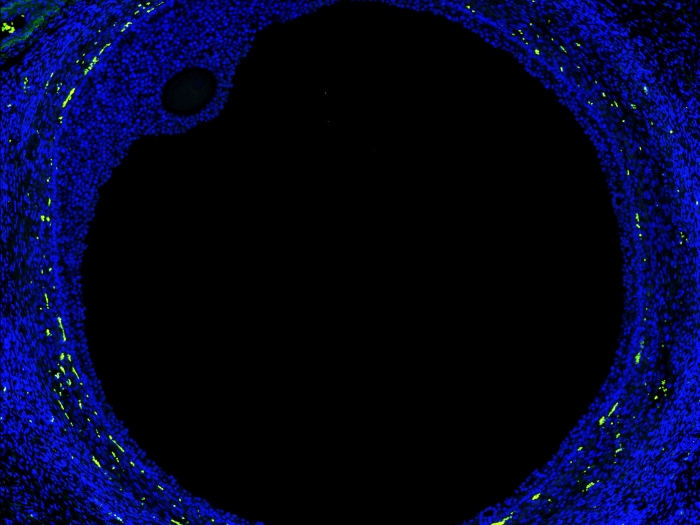
To explain the double role that siderophores play in a K. pneumoniae infection, Bachman and his colleagues had to create bacteria that would not reproduce while still producing siderophores. They were able to mutate bacteria in a way that kept iron-laden siderophores from getting back into the bacterial cells and promoting growth. That way, the number of bacteria in a mouse's body stayed the same, but the researchers could study what the siderophores did.
They expected that if the siderophores grabbed enough iron from the mouse's lung tissue and robbed the mouse of an essential element, the mouse's cells would respond. Indeed, they found that the siderophores triggered the mouse immune system directly, causing the release of molecules called cytokines that attract infection-fighting cells and cause inflammation as a result. The activation of Hif-1alpha was part of this — because the mouse cells sensed that iron supply was low.
So the team figured out how to eliminate Hif-1alpha in the cells lining the mouse lungs — and showed that in these mice, most of the bacteria couldn't escape from the lungs to the spleen. But in mice that made Hif-1alpha, more K. pneumoniae bacteria spread to the rest of the body, making the infection worse.
"This work provides us with motivation to target the production of siderophores, rather than just the uptake of them," says Bachman. "Now that we know that the bacteria cause cellular stress just by secreting them, we may be able to prevent these effects if we neutralize them."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!