Custom medical treatment based on a patient’s biomarkers is a rapidly growing field. How health care systems can keep pace with the progress.
7:00 AM
Author |

Over the past decade, major strides have been made in precision medicine. Analyzing the characteristics or biomarkers of an individual's disease, doctors can personalize treatment using therapeutics that target those biomarkers.
Hundreds of targeted drugs are either in development or already in clinical use to treat cancer and other diseases. Hand in hand with the evaluation and approval of these therapies is the development of molecular tests of blood or tissue needed to identify biomarkers and pair the patient with the most effective, least toxic targeted treatment.
The pace of discovery is rapidly improving tests and treatments; however, regulatory oversight and standards for clinical use and insurance coverage are struggling to keep up.
SEE ALSO: Even with Insurance, Hospital Patients May Pay Over $1,000 for Stay
A recently published report by the National Academies of Sciences, Engineering and Medicine details how biomarker tests are currently being used and assessed. It also suggests a road map to address the "growing pains" of this promising medical frontier.
John Carethers, M.D., chair of internal medicine at the University of Michigan Health System, is a co-author of the report. He discussed the committee's findings and recommendations.
Can you provide a current example of a molecularly based therapy that requires biomarker testing?
Carethers: Here's an example from my specialty, colon cancer: For many years, we have used the drug cetuximab to treat advanced colon cancer. We knew that it worked better for some patients than others, but it wasn't until recently that research advances confirmed the patients who responded best to the drug were those whose tumors had mutations in a gene called KRAS. So now, rather than giving cetuximab to every patient hoping it will work, we first test their tumors for the KRAS mutation.
What are the challenges in offering patients personalized medicine versus traditional treatment?
Carethers: When I prescribe a traditional drug, I'm confident that it's gone through a rigorous FDA review process to ensure it will work as intended — and that its concentration and quality will be consistent.
That's not true in personalized medicine. Biomarker tests are produced by many companies and labs. Some have FDA approval and some do not since right now it isn't mandatory. And even approved tests linked to approved treatments may have been succeeded by more accurate and effective iterations.
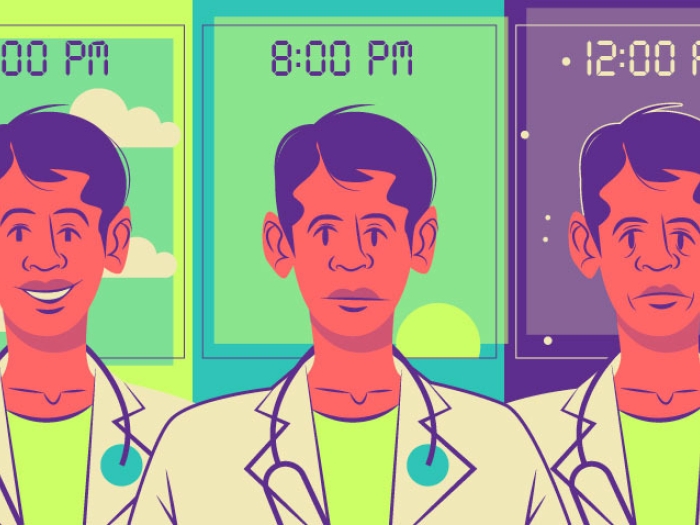
Clinical consistency is just one of the concerns driving this initiative. We're hoping to help the infrastructure catch up with the science. We're seeing an explosion in growth and change in these molecular treatments and corresponding biomarker tests.
As clinicians, it's terrific to have more and better options to offer patients. But we need to feel confident that our recommendations reflect the latest scientific evidence. That's equally true for policymakers, regulators and insurance providers. Right now, there are very few rules to guide us; it's like the Wild West.
Will you summarize your report's recommendations?
Carethers: After interviewing federal regulators, insurers, including those within the Centers for Medicare and Medicaid Services, developers of biomarker tests and members of key advocacy groups like the American Society of Clinical Oncology, we arrived at 10 goals, and recommended that the U.S. Department of Health and Human Services take the lead in moving them forward.
We call for more and better coordinated research on both access to and outcomes of biomarker testing and targeted treatments. That includes studying different demographic and geographic groups, using common standards to evaluate findings and building and maintaining a robust database to coordinate and share what we learn.
We also recommend creating and regularly updating evidence-based guidelines for clinical practice and standards to guide regulatory oversight and insurance practices. In the process, we need to reflect the voices of patients, providers, researchers, test developers, pharmaceutical companies and relevant government agencies.
Finally, we call for standardizing patient- and provider-targeted information and labels to help us all make informed decisions.
That's a tall order. What's the first step?
Carethers: It's a huge undertaking, and perhaps the greatest challenge is that there isn't a single first step. All of the pieces of the puzzle — developing common care standards, streamlining how we collect and share data and advancing regulation and reimbursement policies — must be addressed at the same time.
How does your group suggest moving the field forward?
Carethers: We recommend adopting what's called a rapid learning model. There are several components involved, but it boils down to making sure that everyone in the process is able to learn from how these tests and treatments are performing in the real world.
Obviously, that means being much smarter and swifter and more connected in how we handle data. We need to develop a public database that can house post-approval data — everything learned about the test or treatment once it is in use. Provider sites like the University of Michigan need software updates that allow them to link data from electronic health records with the database. And we need reliable ways to keep regulators and insurers updated.
While it will require tremendous cooperation and coordination, there is precedent for this kind of sea change. More than a decade ago, a nonpartisan working group like ours from the Institute of Medicine published a report called Crossing the Quality Chasm. It made a number of ambitious suggestions for overhauling our health care system, requiring collaboration between players in both the public and private sectors. Among its recommendations was the accelerated adoption of electronic health records. While it hasn't been easy and the results aren't perfect, much progress has been made.
That gives us confidence that we can do the same with precision medicine. Initial feedback from many stakeholders is that this report is a good start.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!