Data-mining medical bills may help protect patients from dangerous complications stemming from medical devices, a U-M team suggests.
9:45 AM
Author |
Every day in operating rooms, diagnostic suites and clinics across America, tens of thousands of patients get medical devices placed in, or connected to, their bodies.
MORE FROM THE LAB: Subscribe to our weekly newsletter
That number has grown rapidly in the past decade with the explosion of new technologies that can find or treat medical issues.
But what if something goes wrong, and a new device doesn't work as planned? What if it harbors a hidden flaw, a hiding place for harmful bacteria or a part that breaks down months after it's in a person's body?
These issues — and the infections, injuries and other medical complications they cause — can go undetected for months or years on a national scale. Problems will only be found if enough reports surface about them in medical circles and the Food and Drug Administration's voluntary reporting system. And some may never come to light in a way that leads to an FDA response or manufacturer recall, if no one can connect the dots between the device and the problems patients' experience.
But University of Michigan surgeon-researchers have an idea how to change that. They've published it in JAMA and presented at AcademyHealth's Annual Research Meeting.
The pair's idea works, as their recent research on a bariatric surgery device shows, as long as Congress follows the recommendations of its members.
How? Through the massive amounts of data that doctors and hospitals already generate about each patient, which is now used to bill for care.
Codes for all devices
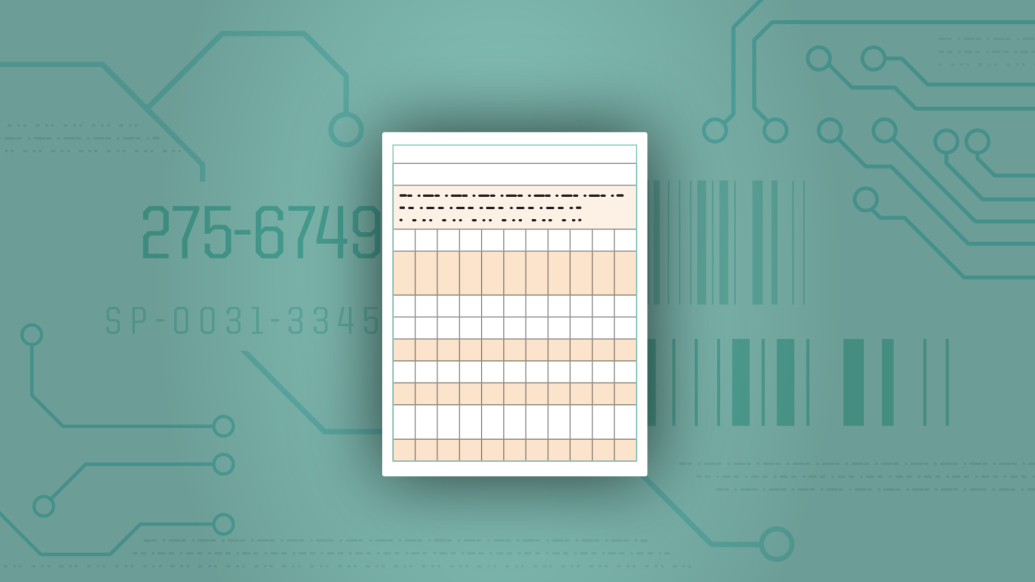
If the FDA assigned a unique code for each device it approves, researchers say, that would make it possible for each use of a device to be tracked in the universal system for billing for medical procedures.
Researchers and regulators could mine this administrative data to look for patterns of problems among patients treated with each device.
"These data, based on ICD and CPT codes, are more comprehensive than voluntary reports about device-related hospitalizations and complications because they are required for reimbursement," says Andrew Ibrahim, M.D., M.Sc., an author of the new JAMA piece. "We envision automatic algorithms that use these codes to find early warning signs and greatly reduce the time it takes to become aware of a new issue."
Even crude measures, such as payments for device removal, could give us valuable signals about safety.Andrew Ibrahim, M.D., M.Sc.
The test case: gastric bands
Ibrahim and his colleague Justin Dimick, M.D., M.P.H., recently published data on the safety of one of the few devices that actually have a unique ICD code: gastric bands used in one form of laparoscopic bariatric surgery.
SEE ALSO: Probing Problems with Bariatric Surgery: Reoperation, Variation Common
Because hospitals and doctors bill for this particular type of surgery using distinct ICD codes to place the device, and a different set of ICD codes to replace or remove it, the researchers could examine billing data and determine how many patients required a device-related reoperation.
They found that nearly 1 in 5 of the 25,000 patients studied had at least one more device-related operation later on, either to remove or replace the band around the upper portion of their stomach or to switch to a different stomach-remodeling approach.
Such data from administrative claims has often been underutilized when evaluating medical devices. For example, in 2011, when the FDA expanded use of the gastric band device, they cited smaller clinical trials demonstrating reoperation rates as low as 4 percent.
Looking back now, Ibrahim and Dimick observed that in 2011 administrative claims from across the whole country for reoperations made up more than 50 of device-related spending. Having such data available to the FDA could vastly improve their ability to evaluate how well approved devices are performing after broad adoption.
"Even crude measures, such as payments for device removal, could give us valuable signals about safety," Ibrahim says of the potential for use of this approach in other types of care.
Making the case
Senior author Dimick, who directs the U-M Center for Healthcare Outcomes and Policy, notes, "We have been using administrative claims data for decades to evaluate and understand nearly all aspects of healthcare in the United States. We are long overdue to take advantage of claims data to help the FDA monitor medical devices."
Ibrahim notes that the U.S. Senate's Health, Education, Labor and Pensions Committee in 2016 called for just that step to be taken, in a report about duodenoscopes, which doctors thread through patients' throats and digestive systems to diagnose issues in the pancreas and bile duct.
These devices were linked to bacterial infection risks not prevented during regular scope-cleaning processes. Because the scopes were used on multiple patients, bacteria from one patient were transmitted to others.
Two hospitals flagged the issue after they noticed illnesses in their patients who had been examined with the scopes. But, said the Senate committee's report, "it took 17 more months for duodenoscope manufacturers and the FDA to alert hospitals, doctors and the public to the risk posed by the devices."
The committee recommended that unique identification codes trackable in administrative claims data and medical records be issued for devices, and that hospitals be required to report device-related issues to the FDA if they want Medicare reimbursement.
What's next
In addition to spotting unforeseen issues like this, unique codes could help researchers study what happens after a device enters the market, says Ibrahim, who is completing a Robert Wood Johnson Clinical Scholars fellowship at U-M. Both he and Dimick are members of the U-M Institute for Healthcare Policy and Innovation.
SEE ALSO: How 'Training' Patients for Surgery Shortens Hospital Stays and Saves Money
The FDA usually approves devices based on positive data from clinical research involving a relatively small number of patients, who were often only treated at major academic hospitals whose teams have extensive experience with the disease or procedure.
But once a device begins is widely adopted, no one is tracking in an independent way whether patients get the same good results as the patients in the clinical trials that led to the device's approval.
Implementing unique codes for devices will take action by Congress, Ibrahim says. Until then, the current system of voluntary reports, recalls — and the threat of legal action by patients who have been harmed — is the only thing protecting Americans from harmful devices.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!