Neurosurgeons want the quickest, most accurate information to help them make decisions during brain tumor surgery. A new method could accelerate that process.
11:00 AM
Author |
A new approach to the practice of surgical pathology for brain tumor patients could make for a powerful combination: more accurate, safer and more efficient operations.
MORE FROM THE LAB: Subscribe to our weekly newsletter
Neurosurgeons and pathologists at Michigan Medicine are the first to execute stimulated Raman histology (SRH), a method that improves speed and diagnostic efficiency, in an operating room. They detail the advance in a new Nature Biomedical Engineering paper.
The researchers imaged tissue from 101 neurosurgical patients using conventional methods and the new method. Both techniques produced accurate results, they found, but the new method was much faster.
SRH, if applied widely, could change the pace and structure of an operation.
"By achieving excellent image quality in fresh tissues, we're able to make a diagnosis during surgery," says first author Daniel A. Orringer, M.D., assistant professor of neurosurgery at the University of Michigan Medical School. "This eliminates the lengthy process of sending tissues out of the OR for processing and interpretation."
Today's workflow for determining a diagnosis during an operation requires the surgeon wait 30 to 40 minutes while tissue is sent to a pathology lab for processing, sectioning, staining, mounting and interpretation. The entire team in the operating room may be idle while waiting for pathology results, Orringer says.
Using SRH also would save money.
"Our technique may disrupt the intraoperative diagnosis process in a great way, reducing it from a 30-minute process to about three minutes," Orringer says. "Initially, we developed this technology as a means of helping surgeons detect microscopic tumor, but we found the technology was capable of much more than guiding surgery."
Near-perfect agreement
Stimulated Raman scattering microscopy, the technology behind SRH, was developed in 2008, but the hazardous lasers involved made it unsuitable for use in an operating room. A clinical version has now been developed and tested in the operating room for more than a year at U-M, with the fiber-laser-based microscope mounted onto a clinical cart that plugs into the wall.
SEE ALSO: Seeing Tumor Tissue Under a Better Microscope
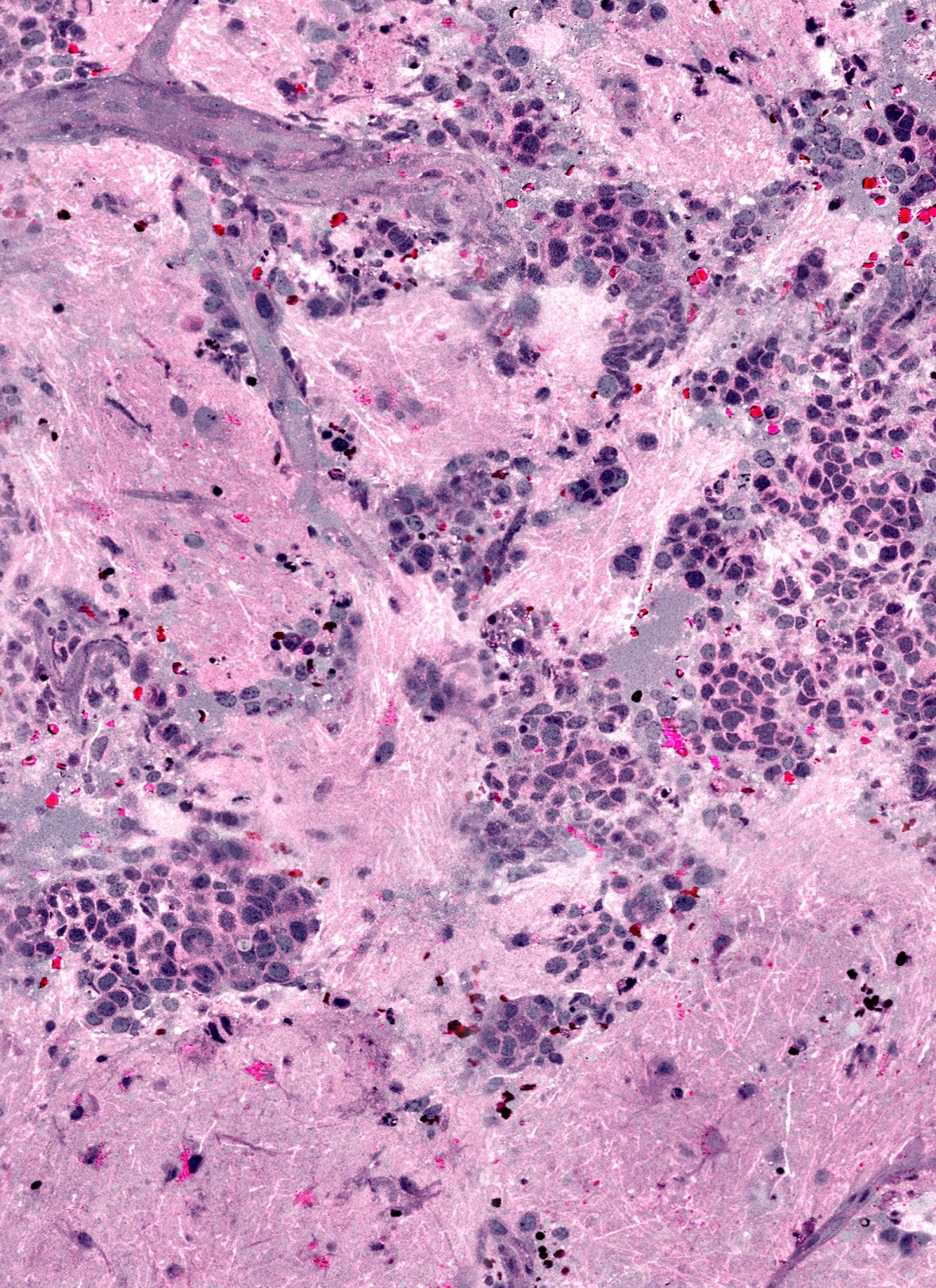
To interpret the samples, researchers developed SRH, which creates images similar to those currently in use.
SRH uses virtual coloring to highlight the cellular and architectural features of brain tumors, with a result resembling traditional staining. The pathologist is then able to differentiate the tumor tissue from normal brain as usual.
"It's very similar to what we currently do in our intraoperative diagnosis, with the exception that the tissue is fresh, has not been processed or stained," says senior author Sandra Camelo-Piragua, M.D., assistant professor of pathology at U-M.
In the Nature Biomedical Engineering study, neuropathologists were given 30 specimen samples processed by SRH or traditional methods. They were told the same information about each patient's medical history and the location of the tumor and asked to make a diagnosis.
Those pathologists, the U-M researchers found, were equally likely to make a correct diagnosis, whether they used SRH or conventional slides.
"SRH imaging will ensure that appropriate and good-quality tissue is collected to reach our ultimate goal: accurate diagnosis," Camelo-Piragua says.
Artificial intelligence
As Orringer and his team improve this imaging technology, they're also teaching a computer how to use SRH images to make diagnoses.
The team built and validated a machine-learning process that was able to predict brain tumor subtype with 90 percent accuracy in a subset of 30 patient samples.
"The more we feed the computer, the more accurate its diagnoses will become," Orringer says.
Connecting hospitals
Using SRH might also improve the workflow for facilities without access to expert neuropathologists. Orringer notes that smaller hospitals may be able to partner with larger systems that do have access, since there are fewer than 800 board-certified neuropathologists but about 1,400 U.S. institutions performing brain surgery.
"Bringing the SRH to smaller hospitals would extend their capabilities, because the images can be interpreted remotely," he says. Sample preparation is minimal, and the SRH could quickly deliver virtual histologic sections to aid diagnosis remotely.
The next step is a large-scale clinical trial, with a goal of showing equivalence between conventional methods and the SRH technique for making diagnoses, Orringer says. The prototype system is intended for research use only.
Disclosure: Daniel A. Orringer, M.D., and co-author X. Sunney Xie, Ph.D., are advisers and shareholders of Invenio Imaging Inc., a company developing stimulated Raman scattering microscopy systems. Co-author Christian W. Freudiger, Ph.D., is an employee and shareholder of Invenio Imaging, Inc.
The University of Michigan, Harvard University and Invenio Imaging have intellectual property used in this research.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!