New technology — a device called EndoFLIP — offers a more complete view of digestive disease than existing diagnostic procedures.
8:00 AM
Author |
A technology known as EndoFLIP® (endolumenal functional lumen imaging probe) is a newer, minimally invasive device created to complement traditional diagnostic tests, such as high resolution esophageal manometry and barium esophagram.
Both of the traditional diagnostic tests are useful in most cases. The esophagram visually demonstrates the clearance of the bolus — swallowed material — from the esophagus. And while manometry measures the strength of contraction in the esophagus, the probe is very thin and may not accurately represent the mechanics of the esophagus in response to a bolus of food.
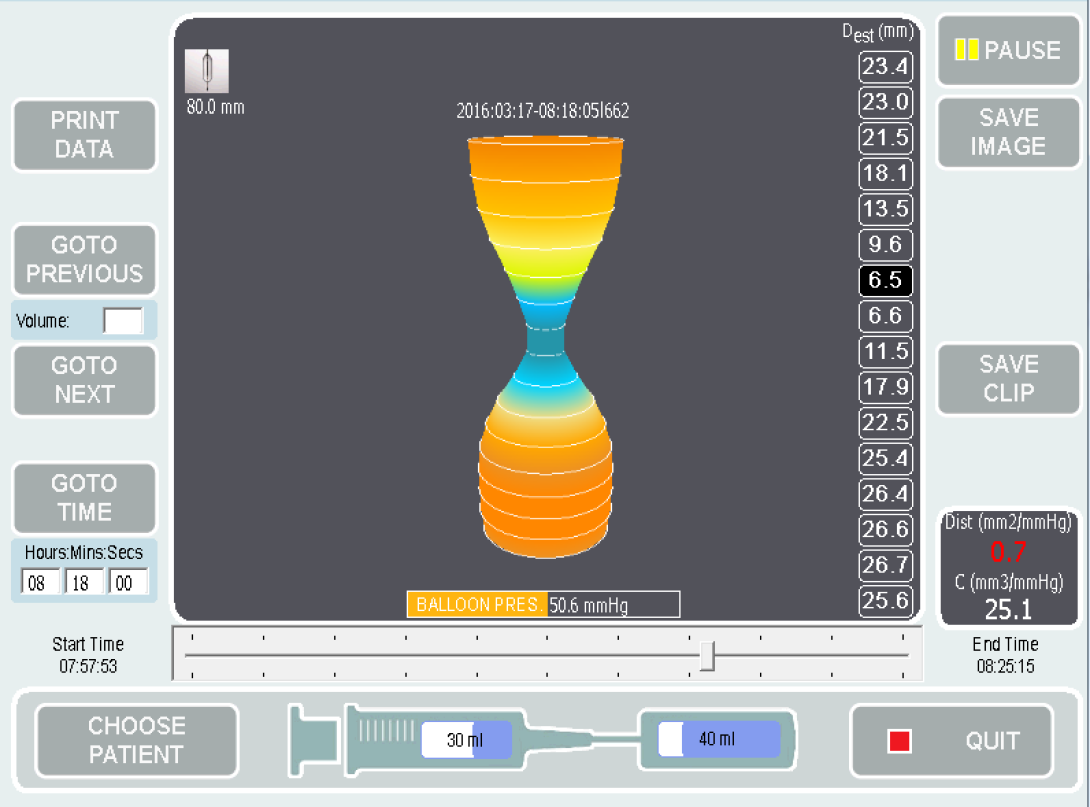
EndoFLIP uses a balloon mounted on a thin catheter placed transorally at the time of a sedated endoscopy. In comparison to the traditional diagnostic tests, EndoFLIP offers the additional capability of measuring the cross-sectional area and intraluminal pressure of the esophagus while under distension (as if a solid bolus was present). The technology uses impedance planimetry to estimate cross-sectional area.
The University of Michigan Esophageal Disorders Program is one of a handful of centers in the region with experts trained to use this EndoFLIP technology. Our first EndoFLIP procedure took place this past winter.
Here are some things doctors should know:
How it works
During an upper endoscopy (EGD), a catheter is passed transorally into the stomach. A balloon attached to the catheter is inflated with a specific concentration of solution with known ionic properties to various volumes.
A small electrical current is passed through an electrode located on the catheter inside the balloon. The current can only pass to its paired electrode through the solution in the balloon. The voltage gradient between the pair of electrodes is inversely proportional to the cross-sectional area at the midpoint between the pair of electrodes.
The catheter has multiple pairs of electrodes along its length which are sequentially activated.
Simultaneously, the pressure in the balloon is measured. Software calculates the distensibility index (the ratio of the cross-sectional area to the pressure). Data is manually reviewed after the procedure.
How it feels
From the patient's perspective, a diagnostic EndoFLIP procedure feels just like an EGD. EndoFLIP can also be used therapeutically to provide pneumatic dilation for achalasia — a specific condition where the lower esophageal sphincter fails to relax to permit passage of the bolus, causing difficulty swallowing — without using the traditional method, which necessitates radiation exposure by fluoroscopy.
The EndoFLIP is particularly helpful in cases where the findings on manometry and esophagram are discordant for an achalasia diagnosis. It may also be helpful in achalasia patients who have a recurrence after treatment — EndoFLIP is useful in determining whether a repeat procedure directed at the lower esophageal sphincter would be beneficial for the patient or not.
We presented our results of a systematic review at Digestive Diseases Week 2015 on what thresholds of distensibility of the esophagogastric junction should be used for diagnosing achalasia.
Importantly, we found that the distensibility of the esophagogastric junction in patients following successful fundoplication for GERD is similar to that in patients with achalasia. This means that the distensibility of the esophagogastric junction needs to be interpreted in the context of the demonstrated motility of the body of the esophagus. This highlights the clinical pearl that patients being considered for fundoplication for regurgitation symptoms should routinely undergo esophageal manometry pre-operatively to exclude aperistalsis in the body of the esophagus, as such patients would be at high risk for dysphagia following fundoplication.
Going forward
In the future, we hope that EndoFLIP may be able to distinguish phenotypes of achalasia or other dysmotilities that can help guide specific management.
For now, we will continue to use EndoFLIP as a diagnostic tool and to deliver pneumatic dilation without the need for exposing the patient to fluoroscopy.

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!